Throughout its history of more than 75 years, VA has funded critical research that has led to many medical advancements instrumental to the agency’s primary goal: to honor America’s Veterans by providing exceptional health care that improves their health and well-being. At the same time, a stream of VA researchers, physicians and scientists have pioneered groundbreaking innovations, with some earning such prestigious honors as the Nobel Prize and the Albert Lasker award, among other national and international recognition.
The following is a list of 12 men and women who have added prestige to VA with their pioneering work, as well as examples of how VA research has impacted everyday health care within VA and in medical care in general:
Dr. Oscar Auerbach
VA New Jersey Health Care System
Main area of study: lung cancer
Pioneering work in the 1960s at the East Orange VA in New Jersey established the causal link between smoking and lung cancer. The tobacco industry criticized earlier observations linking lung disorders and cigarette smoke. But landmark lab research by Dr. Oscar Auerbach that studied the effects of smoking over a three-year period found that smoking can cause major changes in lungs and even lead to cancer. That VA research led to warning labels on cigarette packages and was cited in the 1964 U.S. Surgeon General report on the dangers of smoking. By studying thousands of slides of human tissue, Auerbach and his colleagues also showed the dangers of second-hand smoke.
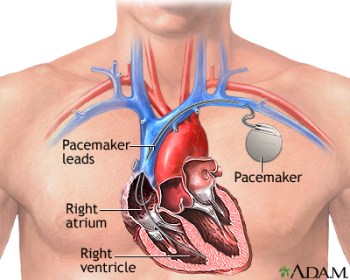
Dr. William Chardack
Buffalo VA Medical Center
Main area of study: cardiothoracic surgery
Did you know that VA researchers invented the first clinically successful cardiac pacemaker? In 1958, Dr. William Chardack, then chief of surgery at the VA hospital in Buffalo, teamed up with engineers to test an early model of their device—basically, an electrode attached to a pulse generator. They refined the design of the unit and, in 1960, implanted pacemakers into a 77-year-old man who lived for 10 months. That year, they implanted pacemakers into nine other patients, some of whom lived for more than 20 years. The design was the first implanted pacemaker to be commercially produced. Implanted cardiac pacemakers prevent life-threatening complications from irregular heartbeats.
Dr. Edward Freis
Washington DC VA Medical Center
Main area of study: hypertension
In the 1960s, VA undertook the first well-designed, placebo-controlled trial to show whether medication can prevent death in those with moderate high blood pressure. The research led to a revolution in the care of people with hypertension. In 1964, Dr. Edward Freis and colleagues launched a VA study on antihypertensive agents. The study showed that drug treatment for moderate high blood pressure reduced patient deaths by over 50%. Previously, high blood pressure was considered a normal part of aging, and it was not known that treating high blood pressure could prevent death. In 1971, Freis received the Albert Lasker award for his groundbreaking work on blood pressure treatment.
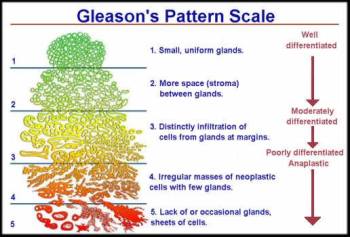
Dr. Donald Gleason
Minneapolis VA Medical Center
Main area of study: prostate cancer
Prostate cancer is the most common cancer in American men, with one in eight being diagnosed with the disease at some point in their lives. A VA pathologist, Dr. Donald Gleason, created a scoring system in the 1960s that is used almost universally today to predict the aggressiveness of prostate cancer. Since Gleason created the scoring system, millions of men have gotten a “Gleason score,” which is considered the most reliable sign of the potential for prostate cancer to grow and spread. It’s also a reference standard in clinical trials for new therapies. Prostate cancer is usually found in its early stages and often grows slowly. Most men live with it for decades and die of other causes even without surgery.
Dr. Millie Hughes-Fulford
San Francisco VA Health Care System
Main area of study: weightlessness, T-cell dysfunction
A VA scientist became the first female payload specialist to take part in a NASA mission. Dr. Millie Hughes-Fulford, a molecular biologist, flew aboard the shuttle Columbia in 1991. She conducted experiments on the effects of space travel on humans, research that shaped the rest of her career. In VA, she studied the effects of space flight on bone and t-cell dysfunction. T cells are important white blood cells of the immune system and play a key role in immune response. In all, she contributed to more than 120 papers and abstracts on t-cell activation and bone and cancer growth, research that benefited astronauts, Veterans and others.
Dr. Ludwig Gross
James J. Peters VA Medical Center (Bronx, NY)
Main area of study: virally transmissible cancer
Longtime VA scientist Dr. Ludwig Gross was a pioneer in cancer research and the father of modern retrovirology. Gross, who served in the U.S. Army Medical Corps during World War II, discovered the first two mammalian cancer viruses in the 1950s. He also was the first scientist to show that leukemia in mammals was transmitted by a virus. Some scientists questioned whether viruses could cause a disease as complex as cancer. But other scientists, inspired by his experiments, reached similar conclusions. In 1974, Gross received the Albert Lasker award for his discovery of what became known as the gross mouse leukemia virus.
Dr. William S. Middleton
William S. Middleton Memorial Veterans Hospital
Main area of study: internal medicine
Dr. William S. Middleton, a renowned internist and military physician, served as VA’s chief medical director from 1955 to 1963. He led the development of Veterans’ programs that included improved access to physical rehab services, mental health care and treatment for heart diseases. Today, the William S. Middleton award is one of VA’s most prestigious scientific awards. It honors VA scientists for their achievements in biomedical and bio-behavioral research relevant to the health care of Veterans. Middleton award recipients have earned international acclaim, and a VA hospital in Wisconsin bears Middleton’s name as the William S. Middleton Memorial Veterans Hospital.
Dr. William Henry Oldendorf
VA Greater Los Angeles Healthcare System
Main area of study: neurology, medical imaging
Dr. William Henry Oldendorf, a VA physician and researcher, originated the technique called the CT scan, a method for making multiple X-ray images of the body or parts of the body. He’s also credited with pioneering the theory behind other forms of medical imaging. Oldendorf was a neurologist at the Los Angeles VA in the 1950s when he received a $3,000 grant to pursue his research. He used some of the money to build a prototype of a CT scanner in his home, using, among other things, tracks from a model train set. In 1975, he received the Albert Lasker award for revolutionizing the field of medical diagnosis though the CT scan. He was also nominated for a Nobel Prize.
Dr. Andrew Schally
Miami VA Medical Center
Main area of study: endocrinology
Longtime VA scientist Dr. Andrew Schally is a pioneer in understanding endocrine signaling in the nervous system. The endocrine system relates to glands that secrete hormones or other products into the blood. In endocrine signaling, a cell targets a distant cell through the bloodstream. In 1977, Schally won the Nobel Prize for discovering that the hypothalamus links the nervous system to the endocrine system via the pituitary gland. That gland controls metabolism, growth, sexual maturation, reproduction, blood pressure and many other key physical functions and processes. Although much of Schally’s work has focused on cancer, he’s made landmark contributions in other fields, such as gene therapy, and he’s authored more than 2,400 scientific papers.
Dr. Thomas Starzl
Denver VA Medical Center
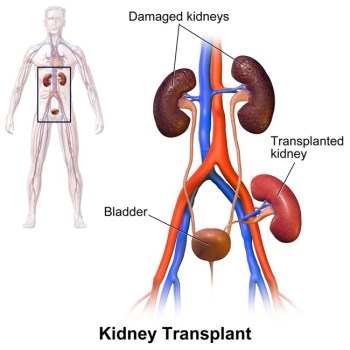
Main area of study: transplantation
Longtime VA transplant surgeon and research scientist Thomas Starzl is widely regarded as the “father of transplantation.” Although not the first surgeon to perform a successful kidney transplant, he’s credited with the “first-ever series of repetitively successful human kidney” transplants. They resulted in long-term survival for patients. He carried out the first of those in 1962. He’s also credited with performing the first successful liver transplant in 1963. While Starzl’s patient succumbed to pneumonia weeks after the liver transplant, it was still considered a huge success and paved the way for life-saving procedures for many others.
Dr. Rosalyn Yalow
James J. Peters VA Medical Center (Bronx, NY)
Main area of study: radioimmunoassay
Dr. Solomon Berson
James J. Peters VA Medical Center (Bronx, NY)
Main area of study: radioimmunoassay
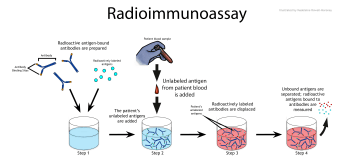
Radioimmunoassay is a sensitive method for measuring small amounts of a substance in the blood—and is widely used today. It measures levels of hormones, viruses, enzymes and many other substances. Two VA researchers, Dr. Rosalyn Yalow and Dr. Solomon Berson, developed the technique. They published a report on it in 1960. Yalow received a Nobel Prize in 1977. Berson, who died in 1972, wasn’t eligible for the Nobel, which is not awarded posthumously. The two also published a paper on how the body uses insulin. They showed that type 2 diabetes is caused by inefficient use of insulin, instead of a lack of insulin.
Topics in this story
More Stories
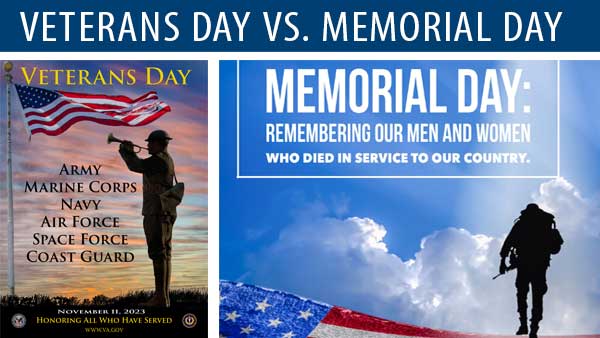
Memorial Day, which is observed on the last Monday in May, was originally set aside as a day for remembering and honoring military personnel who died in the service of their country, particularly those who died in battle or as a result of wounds sustained in battle.
Diverse representation of women in health care research allows MVP to make discoveries for women’s health
Join the Million Veteran Program online. You will have the option to receive an at-home blood sample collection kit in the mail.











These were all amazing stories about VA researchers! Great read.
Waste of taxpayer money(. How many Veteran families suffered while “Agent Orange” R&D continued at delayed pace. CHildren!!! How many years between Korea and Vietnam? 7,000+ years acupuncture in use world wide but not at VA because the “slow do R&D and continue with their marriage to drug industry? Suicidal issue advancement??! Oh, how great thy are