 Ever since Sir Alexander Fleming discovered penicillin nearly 90 years ago, antibiotics have been a powerful means for treating bacterial infections and saving lives. Unfortunately, prescribing practices around these drugs have resulted in “antibiotic resistance.” Whether it’s the use of antibiotics without testing to first confirm infection, improper dosing, or poor communication with patients regarding compliance, the end result is the same. Many antibiotics are no longer effective at killing the bacteria they once killed, making it difficult, if not impossible for doctors to treat certain infections.
Ever since Sir Alexander Fleming discovered penicillin nearly 90 years ago, antibiotics have been a powerful means for treating bacterial infections and saving lives. Unfortunately, prescribing practices around these drugs have resulted in “antibiotic resistance.” Whether it’s the use of antibiotics without testing to first confirm infection, improper dosing, or poor communication with patients regarding compliance, the end result is the same. Many antibiotics are no longer effective at killing the bacteria they once killed, making it difficult, if not impossible for doctors to treat certain infections.
To ensure antibiotics remain effective, we all play a role – doctors, hospitals and patients. While the first line of defense is to prevent infection, there are also some key points to keep in mind when using antibiotics.
First, don’t ask for antibiotics when you have a virus such as a cold or flu. Antibiotics don’t work on these infections.
Next, only use antibiotics when your health care provider prescribes them for you, and follow the directions when taking them.
Finally, be sure to finish the entire course of antibiotics – even if you start to feel better – to ensure the infection is fully gone.
Antibiotic resistance can also lead to adverse drug reactions – allergic reaction, antibiotic drug toxicities and more – or complications that make patients even sicker, require hospitalization, prolong hospitalization and create a higher risk of death from infection.
According to the Centers for Disease Control and Prevention (CDC), nearly half of all hospitalized patients are given an antibiotic for at least one day of their hospital stay.
That is an alarming statistic, which should worry us, whether we’re clinicians, hospital administrators or patients.
Could testing have determined if the drug was needed in the first place? Did the patient understand the dosing instructions, including the importance of taking the entire prescription even if their symptoms cleared up?
Because of this, antimicrobial stewardship programs have become a top priority for hospital and healthcare systems nationwide. These programs seek to prescribe appropriately, provide for regular reassessment, and closely monitor patient outcomes, among other goals.
The CDC recently recognized VA’s efforts in antimicrobial stewardship. Our National Antimicrobial Stewardship Task Force (ASTF), chartered three years ago, oversees a number of activities, including six work groups, monthly educational conferences and the collection and dissemination of a wide variety of resources for VA field offices to use in developing local stewardship policies. As of November 2012, 64 percent of VA facilities had an antimicrobial stewardship policy in existence or in development. Earlier this year, we reaffirmed our commitment to antimicrobial stewardship through the development and publication of VHA Directive 1031 . Importantly, this directive establishes stewardship programs in all VA facilities by the end of this coming July.
Up to now, the ASTF has focused primarily on stewardship initiatives for hospital settings and is now seeking to develop similar initiatives for outpatient settings and long-term care facilities such as Community Living Centers. We’ve also worked closely with VA’s Office of Research and Development, to develop a solid evidence-base for new practices and policies. You’ll be hearing more about the VA’s Antimicrobial Stewardship Program in the coming months. For more information about antimicrobial stewardship, visit the CDC’s “Get Smart for Healthcare” at www.cdc.gov/getsmart/healthcare/


Topics in this story
More Stories
Summer can be a joyful time of year, but some outdoor activities can be hard for some Veterans. In this guest post, former VA Secretary Bob McDonald shares resources and plans to navigate summer activities.
"A CAPITOL FOURTH" airs on PBS Thursday, July 4, 2024 from 8:00 to 9:30 p.m. E.T.
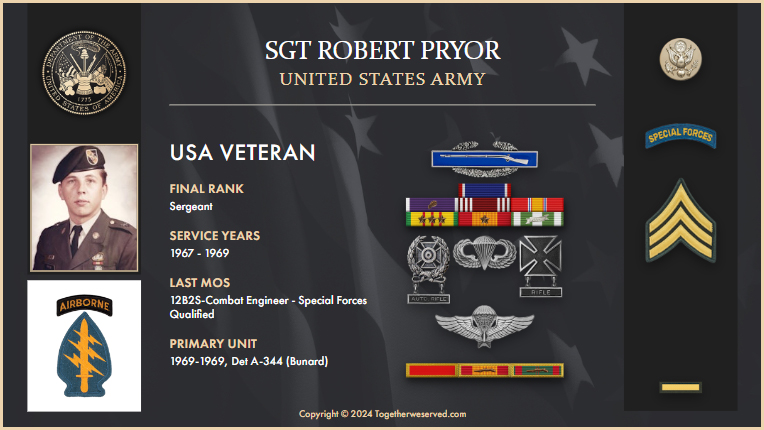
The following is an account from Army Veteran Robert Pryor on how he was able to find and reconnect with the pilot who saved his life in Vietnam.






“First, don’t ask for antibiotics when you have a virus such as a cold or flu.” Then two paragraphs later the article states, “…..finish the entire course of antibiotics – even if you start to feel better – to ensure the virus is fully gone.”
I believe the doctors meant, “to ensure the (bacterial) infection is fully gone.”
Thanks for the catch, Dan!