 “We can’t make the traumatic memory in your head go away. But we might be able to take away the intense emotions associated with that memory, so that it’s simply a memory and no longer upsetting.”
“We can’t make the traumatic memory in your head go away. But we might be able to take away the intense emotions associated with that memory, so that it’s simply a memory and no longer upsetting.”
That’s according to Dr. Alina Suris, chief of psychology at VA North Texas Health Care System in Dallas, and could be a critical first step in dealing with the triggers for post-traumatic stress.
Suris and her team of researchers have conducted some preliminary studies in which they’ve successfully interfered with traumatic memories at the cellular level. However, she emphasized that her research, while promising, is still in its infancy.
“We’re not erasing memories,” she explained. “We’re quieting the emotions associated with those memories. You’ll still have the memory… but your emotional response to that memory won’t be so overwhelming or debilitating.”
Anywhere from 11 to 20 percent of Iraq and Afghanistan Veterans develop PTS symptoms, according to VA estimates. These include flashbacks, nightmares, depression, social withdrawal, emotional numbing, hyper-alertness, anxiety and irritability.
“Traumatic memories can be ‘cued’ at any time,” Suris continued. “You’ll see something on TV. Or you’ll see a green Army truck going down the street. When a traumatic memory is triggered, something happens at the cellular level. There’s a chemical response that involves cortisol.”
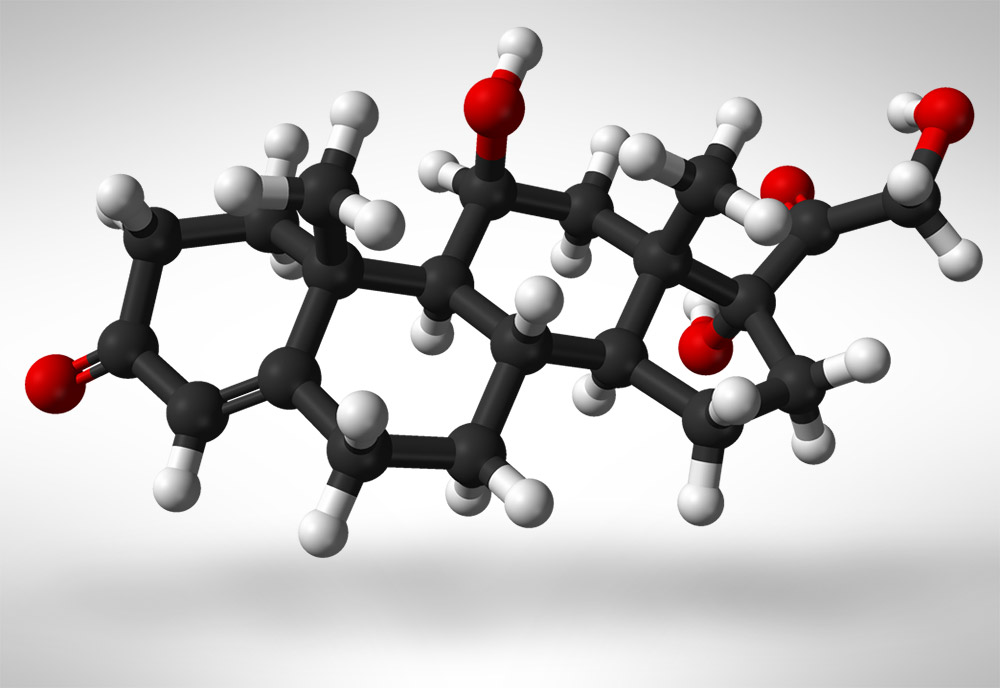
Cortisol, known more formally as hydrocortisone, is a steroid hormone. It is released by the body in response to stress. “Your heart may start to race,” Suris said. “Your palms may get sweaty. A panic may begin to rise up inside you.”

Dr. Alina Suris is chief of psychology at VA North Texas Health Care System in Dallas,
“But what if we could interfere with that chemical response?” she asked. “What if we could intercept it before it really gets going?”
During her preliminary research, Suris and her team asked Veterans to write down their most traumatic battlefield experiences. Once a Veteran captured his most terrifying experience on paper, researchers edited it down into a 30-second script.
During a follow-up visit, the Veterans were asked to relax in a comfortable recliner. Each Veteran was then given either a steroid pill or a placebo pill. After the medication was given a chance to work, they listened while a narrator recited their 30-second script to them.
“We know that Veterans with PTSD have trouble mounting a cortisol defense to help them deal with memories that get triggered by certain cues,” Suris said. “We believe that by giving oral steroids, we may be able to supplement what the body needs to handle the trauma memories in a more healthy way.”
The results have been encouraging.
“During our follow-up assessments, those Veterans who received the steroid expressed significantly fewer PTSD symptoms,” Suris reported, “while those who were given a placebo continued to have significant symptoms such as avoiding places, people, activities or thoughts that remind them of their trauma.”
Currently, the two most common therapies for treating PTSD are Cognitive Processing Therapy and Prolonged Exposure Therapy.
“These are good, evidence-based therapies,” Suris said. “They work. They are the best we have right now.”
The current research seeks a treatment that is just as effective. “It would be quick, efficient, and economical. Most important, it would likely be more palatable to Veterans because of significantly less demand on their time in therapy,” Suris said.
“Our Veterans deserve the best we can offer them,” she added. “That’s why we invest heavily in research here at VA and are constantly looking for ways to improve the care we provide.”
To learn more about how VA is helping Veterans with PTSD, visit www.ptsd.va.gov.
Topics in this story
More Stories
The Social Security Administration is hoping to make applying for Supplemental Security Income (SSI) a whole lot easier, announcing it will start offering online, streamlined applications for some applicants.
Yusuf Henriques, an Army Veteran and former combat medic, is the founder and CEO of IndyGeneUS AI, a genomics company on a mission to improve health equity by increasing representation of women and racial minorities in clinical trials.
Online shopping scams are the riskiest scam for Veterans, with 77.3% of reports confirmed losing money when targeted by this scam.







The problem is the more evil you see and the more your eyes are opened you can never close them again. The bad memories and experiences serve as a filter forever for the future. Think locally and act locally is my motto. Focus on your own little world and make it perfect and forget what goes on “out there”
The experience I had as a Vietnam Combat Veteran is that my memories became my psychosis. That means, for 30-years I was still in Vietnam flying combat mission as a Cobra pilot. My dreams were as real as day and I did not know the difference. I would always ask if I were awake or asleep because they both felt the same. I had to learn a new skill to break my psychotic connection to live a somewhat normal life. Today, my traumatic memories are no longer traumatic.
An interesting concept – provided the person actually remembers the trauma event. There are some of us who know we have been in combat situations, yes have no conscious memory of it. For example, there may be several blocks of time in memory that are totally blank to the conscious mind – yet we know something happened because of evidence from other people, and PTS related events in everyday life (anxiety, nightmares, depression, startle responses, flashbacks and so on.) In a way not being able to remember may be a benefit, but another consideration is if that is actually hindering treatment. Would it be a benefit if a person was to be able to remember events while being prepared for the possible trauma?
My non professional opinion is that it would not help with repressed memories. That road-block has to be removed first. Generally repression is “used” when the mind is doing an attempt to protect itself from certain knowledge or more than it can handle. Getting yourself to a safe, stable, supported place to begin the remembering, which will be tough to go through, might be your first priority.
thank you so much for that comment! I am a non combat veteran diagnose 100%service related PTSD. I often feel guilty because of my diagnosis yet I have nightmares about being in combat.I actually have abused my wife in the middle of the night while dreaming and she hasn’t found me in the corner in the middle of the night fighting with nobody else in the room. I now have a service dog for my PTSD and she wakes me up when I have these nightmares.all I can say again is it thank you for that comment. as always,God bless our troops God bless our veterans and God bless America!
Why can’t u help veteran out who are in pain . without giving antidepressant . antidepressant drugs give more problems, Dont do the job as a narcotics, its not fair stop veteran cold when their been take and pain meds that help them.
Can you get a second opinion? If pain is NOT all or mostly aches and pains due to psychiatric condition with anti depressants if depression and anti anxiety meds if stress related ( and if you don’t have an addiction history) you might be getting the wrong treatment. Much depends on the injury illness or what is causing the pain and what other non med modalities are available.
Best of luck and health to you !