The Departments of Defense (DoD) and Veterans Affairs today announced its ongoing effort to ease the transition for Servicemembers who require complex care management as they transition from the DoD system of health care to VA or within each system. The effort is designed to ease the burden for service members and Veterans, who have suffered illnesses or injuries so severe as to require the expertise provided by multiple care specialties throughout both departments.
“More than a decade of combat has placed enormous demands on a generation of service members and Veterans – particularly those who have suffered wounds, injuries or illnesses which require a complex plan of care,” said Dr. Karen Guice, Principal Deputy Assistant Secretary of Defense for Health Affairs, and co-chair of the DoD-VA Interagency Care Coordination Committee (IC3). “These individuals require the complex coordination of medical and rehabilitative care, benefits and other services to successfully transition from active duty to Veteran status, and to optimally recover from their illnesses or injuries.”
“Our collaborative efforts with DOD have improved and enhanced the process of caring for our military members with serious illness, injuries or disabilities, as they recover and return to their communities. Great attention has been made to developing a system which focuses on continuity of care, holistic support services and a ‘warm handoff’ for Servicemembers and Veterans as they move from and between military, VA and community health care systems. Our care coordinators now have at their fingertips tools and processes that improve and simplify the lines of communication for our wounded, ill and injured Servicemembers and Veterans who require complex care coordination, their families and those who provide their care in both Departments,” said Dr. Linda Spoonster Schwartz, Assistant Secretary for Policy and Planning for VA, and co-chair of the DoD-VA Interagency Care Coordination Committee (IC3). “This process will enhance and improve the quality of care and services for these Veterans and their families now and in the future.”
The hallmark of the effort is the implementation of the role of lead coordinator. The lead coordinator will be a designated member of a service member’s care management team who will serve as the primary coordinator for that individual. The lead coordinator will offer personal guidance and assist the Servicemember and their family in understanding the benefits and services to which they are entitled. Servicemembers, Veterans, and their families, working with their lead coordinator, will have someone to whom they can turn when they have a question or issue as they actively participate in their care. The first phase of lead coordinator \training was completed in November. It is expected that a total of 1,500 DoD staff and 1,200 VA staff will serve as lead coordinators.
This effort comes as a result of the work of the DoD-VA IC3, established in 2012 to implement a joint, standard model of collaboration for the most complex cases of care that will require a warm handoff from the DoD to the VA system of care, as well as within the departments, and is based on many of the best practices of collaboration that have been created over the last decade. This effort was enacted as policy by both departments in 2015, aligning more than 250 sub-policies to one, overarching policy that will govern the coordination of complex care cases that transition between the two departments.
Coordination efforts are synchronized through the IC3 community of practice, a group representing more than 50 DoD and VA programs that provide specialty care, including rehabilitation services for the visually impaired and polytrauma centers. It will be the job of the lead coordinator to guide Servicemembers through the system, ensuring that they receive the care, benefits and services they both require and to which they are entitled.
Topics in this story
More Stories
On Thursday, June 20, 2024, VA joined more than 20 federal agencies to release its updated 2024-2027 Climate Adaptation Plan.
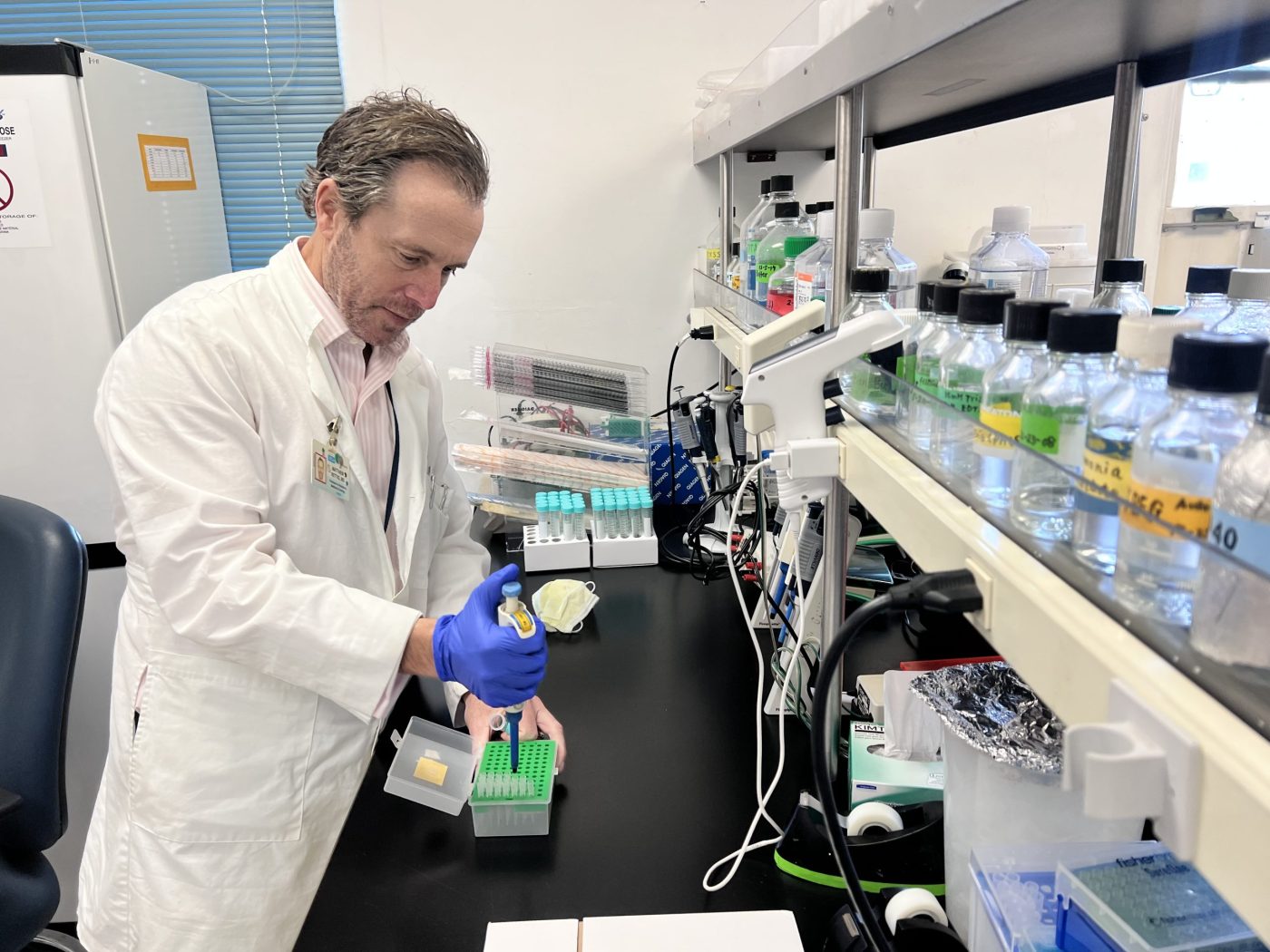
As part of a new research study that began July [...]
WASHINGTON ― The Department of Veterans Affairs Office of Research [...]





Heathnet has to be one of your all time jokes, I have to travel 3 hours roundtrip to get to a clinic, the clinics might as well be called triage centers for as little as they can do or go 8 hour roundtrip to a VAMC to be told I need to make an appointment with Healthnet who still makes appointments at doctors that stopped accepting them up to 9 months before, leaving me to get another appointment8 hours away after another visit to the clinic for another referral from the fist part of December to hopefully next week when I finally get an appointment hopefully this doctor accepts
At the vaMC they do more harm than good pain specialist leaves me on the same medication for 6 years I met with all 3 of the new doctors and as told they were going to cut me off cold turkey instead 9 months later they prescribe physical therapy wich normally tells me it is time for surgery or see a surgeon will it be another 2 year wait
What’s the sense? When I am done leaving my comments, you’re gonna say my code is wrong and it didn’t go through, as you always do! I’ m fed up with trying to address my issues with the VA…plain and simple! But boy, you talk a good game though! See, some of us actually need help!
That is the damn truth. I sent a rather lengthy post about pain meds. When I got through, said the Captcha was wrong and all of my post was gone. I think it is a way of censoring what posts get through. Glad to hear others are experiencing it.
Hello
I’m a CNA and looking for a job in a VA facility. Is there a VA Center in Pittsburg, Pa?
Or surrounding areas near there. I believe there is an Army Center, but need more information.
Please contact me.
Thanks,
Priscilla