VA is partnering with the Department of Defense (DoD) and the National Cancer Institute (NCI) to tailor cancer care for patients based on the genes and proteins associated with their tumors. The tri-agency program will create the nation’s first system in which cancer patients’ tumors are routinely screened for gene and protein information, with the goal of finding targeted therapies for each individual patient. The process will also continually generate new information to boost clinicians’ ability to treat the disease.
This new program, the Applied Proteogenomics Organizational Learning and Outcomes consortium, or APOLLO, is part of the wider national Cancer Moonshot initiative. APOLLO will initially focus on lung cancer in patients at VA and DoD medical centers, with plans to eventually include other forms of cancer. Some 8,000 Veterans are diagnosed with lung cancer each year in the VA system alone.
“APOLLO will create a pipeline to move genetic discoveries from the lab to VA clinics where Veterans receive cutting-edge cancer care,” said VA Secretary Bob McDonald. “This is an example of how we are striving to be an exemplary learning health care system. We are proud to join our federal partners in this exciting initiative, and we expect it will lead to real improvements in the lives of those affected by cancer.”
APOLLO complements other Cancer Moonshot initiatives involving VA. One is a partnership between VA and IBM, in which IBM’s supercomputer Watson will help interpret the results of tumor sequencing by recommending therapies and clinical trials. Also in the works is a partnership between VA and the Department of Energy (DoE), known as MVP CHAMPION (Computational Health Analytics for Medical Precision to Improve Outcomes Now), in which researchers will leverage DoE’s high-capacity computing network to help analyze data from VA’s landmark Million Veteran Program. Prostate cancer is among the health conditions to be targeted in the early phases of that work.
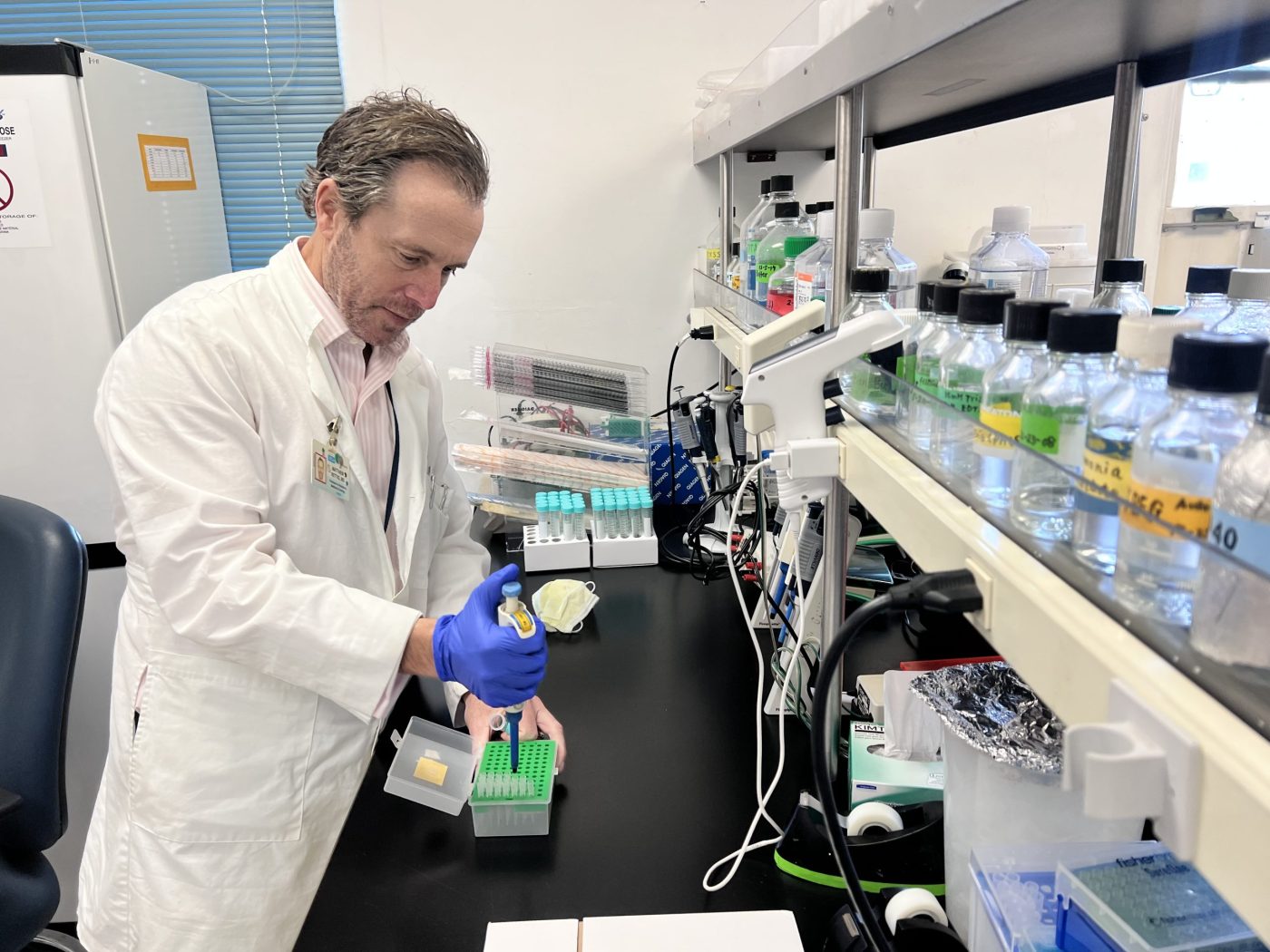
The new effort centers on “proteogenomics”—a blend of genomics (the study of genes and their role in health) and proteomics (the downstream effects of genes), that has recently been demonstrated in NCI’s Clinical Proteomic Tumor Analysis Consortium (CPTAC). CPTAC’s “proteogenomics” approach was successful in demonstrating the scientific benefits of integrating proteomics with genomics to produce a more unified understanding of cancer biology and possibly therapeutic interventions for patients. APOLLO researchers and clinicians will classify Veterans’ lung tumors based on changes in genes in the tumors, and in the levels of proteins. They will use the findings to recommend targeted therapies or refer patients to appropriate clinical trials. The proteogenomics approach promises more precision than looking at genes alone. As the knowledge base grows, it will be widely shared with clinicians and the global cancer community such as through NCI’s Genomic Data Commons to help them learn how to better treat cancer patients in the future.
The APOLLO partnership will leverage the strengths of each agency involved. NCI has cutting-edge expertise in proteogenomics, a relatively new field in science. DoD has a well-established pathology network for receiving and analyzing tissue samples—including DNA and RNA sequencing to identify genes and proteins. VA, as the nation’s largest integrated health care system, offers clinical research expertise and infrastructure plus a large pool of patients with cancer.
Among the benefits of APOLLO are targeted therapy and referrals to clinical trials as part of a larger learning health care system. Once a Veteran’s molecular signature is known—basically, the genes and proteins found in the tumor—he or she could be matched with available clinical trials targeting that signature with an experimental drug.
As part of APOLLO, VA medical centers will expand their participation in NCI’s network of clinical trial sites. They will also partner with other sponsors of clinical trials testing targeted therapies. This will improve Veterans’ access to new therapies through clinical trials.
“A third benefit of APOLLO may be early detection, or even prevention,” said VA Under Secretary for Health David J. Shulkin. “As researchers and clinicians learn more about which gene and protein signatures are associated with cancer, they may be able to do blood tests to screen at-risk patients. Early detection would help ensure treatment is given as soon as possible.”
Topics in this story
More Stories
On Thursday, June 20, 2024, VA joined more than 20 federal agencies to release its updated 2024-2027 Climate Adaptation Plan.
As part of a new research study that began July [...]
WASHINGTON ― The Department of Veterans Affairs Office of Research [...]





I hope the VA will not ignore the needs of female vets with breast and ovarian cancer; so many of us have had to struggle to get our needs met from the day we took the oath to the days of constantly being called “Mrs.” by VA employees who assume a woman has to be a male vet’s wife. We deserve to be respected for our service and we have earned the right to care of the same caliber as our brothers.