More than 700,000 Veterans made more than 2 million telehealth appointments last year. In August, VA Secretary Dr. David Shulkin announced a new initiative that will leverage telehealth and health IT to improve care delivery for our nation’s Veterans. This and other recent efforts by VA seek to use telemedicine as a critical vehicle for improving care coordination and case management, and addressing clinical issues.
Shulkin recently explained that a new regulation will allow VA providers to provide telehealth services to Veterans anywhere around the country: “We call it ‘anywhere to anywhere’ VA health care. That’s a big deal.”
Today, the use of telemedicine has spread rapidly. It is now becoming integrated into the regular operations of hospitals, specialty departments, home health agencies, and private physician offices, as well as consumers’ homes and workplaces. It’s no wonder that this has become a multi-billion-dollar industry: nearly every major hospital and health care system leverages telemedicine to transform and to re-invent how our country approaches health care. More than half of U.S. hospitals use telemedicine to engage with patients remotely – from monitoring vital signs to full-fledged consultations at a distance. Even a basic webcam can allow critically ill patients access to a world-class team of physicians who could be thousands of miles away.
Telemedicine can lower the cost of care while improving outcomes, facilitating efficient decision making and proactive care, and enabling better, more comprehensive patient data monitoring. A prime example of basic telemedicine is using video conferencing to reach patients who otherwise would not be able to see a specialist far from their home. This simple tool can also lead to increased and more effective communication between physician and patient, amounting to higher quality care and reduced costs.
Telemedicine is an important vehicle that can help address barriers preventing rural and Veteran populations from accessing quality care. Telehealth changes the location where health care services are routinely provided, improving the health of and facilitating access to the care that those who have served their country deserve.
As the largest telehealth-focused organization, the American Telemedicine Association (ATA) is a non-profit association based in Washington, D.C., with a membership network of more than 10,000 industry leaders and health care professionals. ATA is a leading the charge to help transform health care by improving the quality, equity and affordability of health care throughout the world. ATA’s strategic focus is to act as a champion for the telemedicine value proposition, empower innovation and change, mobilizing ATA’s resources to effect that transformation.
As the interim CEO of the American Telemedicine Association, I understand how incredibly important these VA telehealth initiatives are for the industry—more importantly for Veterans. These regulations and programs will have lasting impacts for patients, providers, and other industry stakeholders.
ATA takes pride in partnering with trailblazers who are leading the charge in health care transformation—leaders like Secretary Shulkin, who will take the stage at the American Telemedicine Association’s Fall Forum, EDGE 2017, to share the VA’s forward-thinking telehealth strategy.
EDGE 2017 is the foremost access point for health care leaders and innovators in telemedicine, telehealth, and mHealth, and will foster insightful discussions and networking to discover new ways to think about old problems. In coordination with that theme, Shulkin’s keynote address on Oct. 3 will address VA telehealth successes and new initiatives.
About the author: Dr. Sabrina Smith is the interim CEO of the American Telemedicine Association. She has 20 years of progressive and diverse experience in health care and nonprofit management. Smith has worked in academic and not-for-profit health care settings. Before joining ATA, she served as senior vice president for business operations for the Regulatory Affairs Professional Society, a global membership organization of over 12,000 regulatory professionals working in the rapidly growing medical device, pharmaceutical and biotechnology sectors.
Topics in this story
More Stories
Summer can be a joyful time of year, but some outdoor activities can be hard for some Veterans. In this guest post, former VA Secretary Bob McDonald shares resources and plans to navigate summer activities.
"A CAPITOL FOURTH" airs on PBS Thursday, July 4, 2024 from 8:00 to 9:30 p.m. E.T.
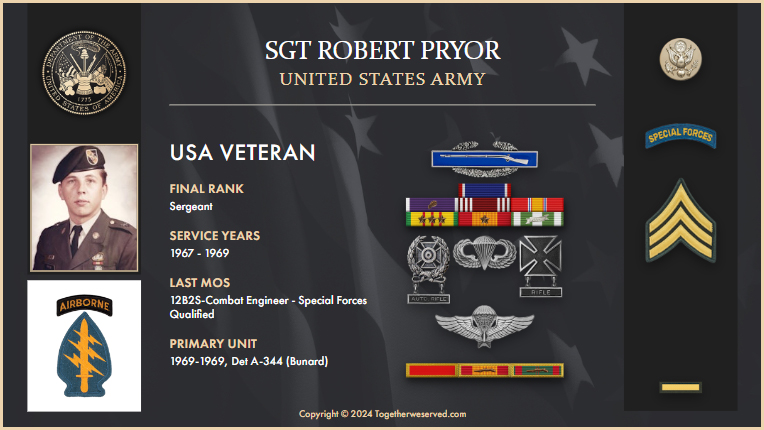
The following is an account from Army Veteran Robert Pryor on how he was able to find and reconnect with the pilot who saved his life in Vietnam.






Thank you for writing this article. I believe this program will be a tremendous help to all Veterans. We are documenting and listing all that has changed under the Trump administration and his accomplishments as President. I’m adding this article to Magapill as one of the changes that has happened with the Veterans Administration.
Every one seems to be soo excited about telehealth.How about the patient’s view? My experiences we’re not good.I arrived at an appointment. No one explained I would be talking to a TV screen, until I walked into an empty room. It was very inpersonal.. I live 30 miles from my V.A. and would rather drive to have a face to face with my Dr’s. I understand it’s use for a homebound patient or one 100 miles away.
I have my temporary Veterans Choice card but no provider in my area will accept it. I live in Crystal Rivers, Fl.
Will this new program help me
My wife can use her Champ card almost any Dr. clinic