Today VA announced a series of immediate actions to improve the timeliness of payments to community providers.
The actions will address the issue of delayed payments head-on and produce sustainable fixes that solve ongoing payment issues that affect Veterans, community providers and other VA partners.
“It is vital to the health of our network of providers that we provide payment in a timely and consistent fashion,” said VA Secretary Dr. David J. Shulkin. “Our outside providers are an essential part of our network and we need to improve our system of payments for their services.”
VA will immediately take the following short and long-term actions to improve payments to community providers. Short-term actions include:
- Publish a list identifying providers with high dollar value of unpaid claims, to be published the week of Jan. 8 at the following website: https://www.va.gov/COMMUNITYCARE/providers/.
- Create rapid response teams to work on the ground with these providers to reach financial settlement within 90 days.
- Increase the number of claims processed by vendors by 300 percent in January 2018 and by 600 percent in April 2018 with a goal of 90 percent clean claims processed in less than 30 days.
- Establish multiple entry points for providers to check the status of their claim, including a dedicated customer service team and VA’s Vendor Inquiry System (VIS) located at https://www.vis.fsc.va.gov.
In addition, long-term actions include:
- Deploy multiple IT improvements within the first six months of 2018 that streamline the claims submission and payment process to reduce time for payments significantly.
- Align on concurrent performance improvement goals with VA’s existing Third Party Administrators to improve multiple aspects of their performance rapidly to ensure Veterans have continued uninterrupted access to care.
- Award four new contracts in 2018 for implementation in 2019 to establish the new Community Care Network that includes elements designed to ensure prompt payment of claims.
- Work with Congress to consolidate and simplify all VA community care programs, including provisions for prompt payment of claims.
- Ensure transparency with VA’s claims processing performance by publishing VA’s claims processing timeliness on a monthly basis.
VA’s current third party administrators, Health Net Federal Services and TriWest Healthcare Alliance, are committed to working with VA to improve the timeliness of payments to community providers. Health Net and TriWest manage VA’s community care networks and process payments to community providers.
“It is an honor and responsibility to serve the Veteran community,” said Billy Maynard, CEO of Health Net. “We remain committed to partnering with VA to improve the claims payment process.”
David McIntyre, president and CEO of TriWest said, “We could not be more pleased at the aggressive focus on this critical topic. We look forward to continuing to reach the industry- leading performance level we all desire and expect.”
Improving timeliness of payments to community providers is a critical element in VA’s goal of building a community care program that is easy to understand, simple to administer and meets the needs of Veterans and their families, community providers and VA staff.
Click here for resources on community care providers. Learn about the new community care network in this video:
Topics in this story
More Stories
On Thursday, June 20, 2024, VA joined more than 20 federal agencies to release its updated 2024-2027 Climate Adaptation Plan.
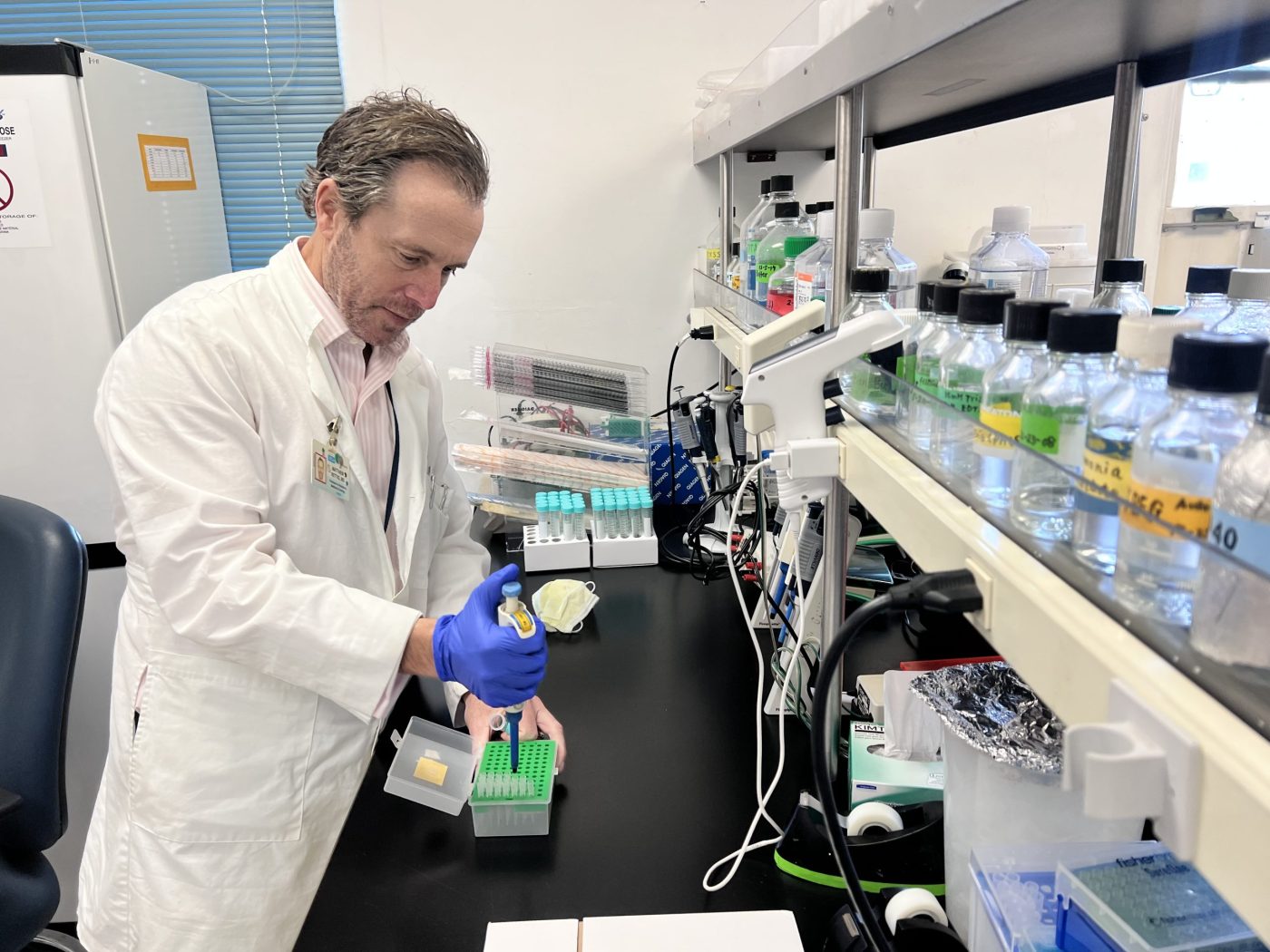
As part of a new research study that began July [...]
WASHINGTON ― The Department of Veterans Affairs Office of Research [...]





I’m going this problem to Jim Costa.
I took an ambulance bill to the Fresno va over a month ago and nothing. Next is Jim Costa.
A little secret, if a GSA approved Vendor submits a bill for payment for products and/or services rendered to Veterans or to the VA and offers a discount for early payment, the VA is required to take advantage of the discount offer and make the payment early. This was how it was when I worked at the VA. So my question is, what happened to this federal policy, why the delay in making payments to vendors, and why the need to create more bureaucracy ??? The “head-on” fix is simple. get the Directors of the VA Medical Centers to get off their collective dead asses. provide the Vendors with information about this policy, and direct the VA Purchasing Dept to make timely payments.