Tim Strebel is no stranger to the spirit of innovation.
Currently a computer programmer focusing on health informatics at the Washington DC VA Medical Center, Strebel has been recognized by VA for his ingenuity.
He’s a two-time winner of the VA “Shark Tank” Award, which honors innovative practices, for developing two software packages to automate the jobs of those who work in prosthetics. The software expedites the billing process for home oxygen users and the ordering of eyeglasses. Both products are used at many VA medical centers. For the eyeglass tool, he also won VA’s Gears of Government Award, which recognizes federal employees and teams whose dedication supports exceptional delivery of key outcomes for the American people.

Strebel, a computer programmer at the DC VA, has earned VA awards for his innovations. (Photo by Robert Turtil)
Now, in what Strebel calls the “most significant” work in his seven-year VA career, he’s developed a tool that uses artificial intelligence to calculate the risk of a COVID-19 patient dying within 120 days of diagnosis. The hope is that clinicians can use those predictions to improve the treatment of their patients. The tool is being piloted at 13 VA medical centers.
Strebel created the tool in collaboration with VA’s National Artificial Intelligence Institute (NAII), which was launched in 2019 to create AI research and development to support Veterans, their families, survivors, and caregivers. He and his colleagues describe the tool in a paper to be published in the journal BMJ Health Care & Informatics.
Artificial intelligence increasingly used in health care
Artificial intelligence (AI) uses computers to simulate human thinking, especially in applications involving large amounts of data. AI is common in the commercial technology sector and is increasingly being used in health care. VA uses AI for purposes such as reducing Veterans’ wait times, identifying Veterans at high risk of suicide, and helping doctors interpret the results of cancer lab tests and choose the best therapies.
Strebel’s tool creates a report that provides AI-generated 120-day mortality risk scores in both inpatient and outpatient settings. The report is based on two models.
The first model assesses conditions about a patient that are known before he or she enters a hospital. It relies heavily on age, body mass index (BMI), and co-existing health conditions that can be found in a Veteran’s electronic health record. Body mass index is a measure of body fat based on one’s height and weight. A high or low BMI may signal health problems.
`But this isn’t practical’
“It’s no surprise that age and BMI are the most predictive factors for mortality in COVID-19 patients,” Strebel says. “An overwhelming amount of concurrent research confirms this. While a few comorbidities on their own are predictive of mortality, such as diabetes and dementia, we’ve found that the amount of and severity of comorbidities in a patient is the best way to use them to predict mortality.”
A second set of models used to predict inpatient mortality considers many of the same factors from the outpatient models, in addition to Veterans’ lab work and vital signs taken at admission. These extra data points “drastically improve” the accuracy of the model, according to Strebel.
“It would be ideal to have this information for every patient diagnosed with COVID-19,” he says. “But this isn’t practical. Bringing every patient in for these tests could increase the risk of transmission and present logistical challenges. That is why we provide the outpatient models to try and provide clinicians with an additional perspective of who may be at risk based on the information we already know about the patient to promote early treatment.”
Age one of the top predictors of death from COVID-19
However, he adds, “One of the biggest challenges in any AI effort is bias. While age is no doubt one of the leading predictors of death, there are always exceptions. Some patients in their 90s survive COVID-19. Conversely, some really young patients die from COVID-19. In those rare cases, our models may show that older Veterans are at higher risk of death than they may actually be simply because of their age. Usually when this is the case, other strong factors such as BUN [blood urea nitrogen] or lymphocytes may be within a healthy range. To help reduce biased decision making, for each of our models we provide additional models that are mirror copies, except we take age out.”
The BUN test measures the amount of nitrogen in a person’s blood that comes from the waste product urea. It indicates how well one’s kidneys are working. Lymphocytes are one of several types of white blood cells, a key part of the immune system.
More Information
Click here to read the full story.
Click here to learn more about VA research.
Topics in this story
More Stories
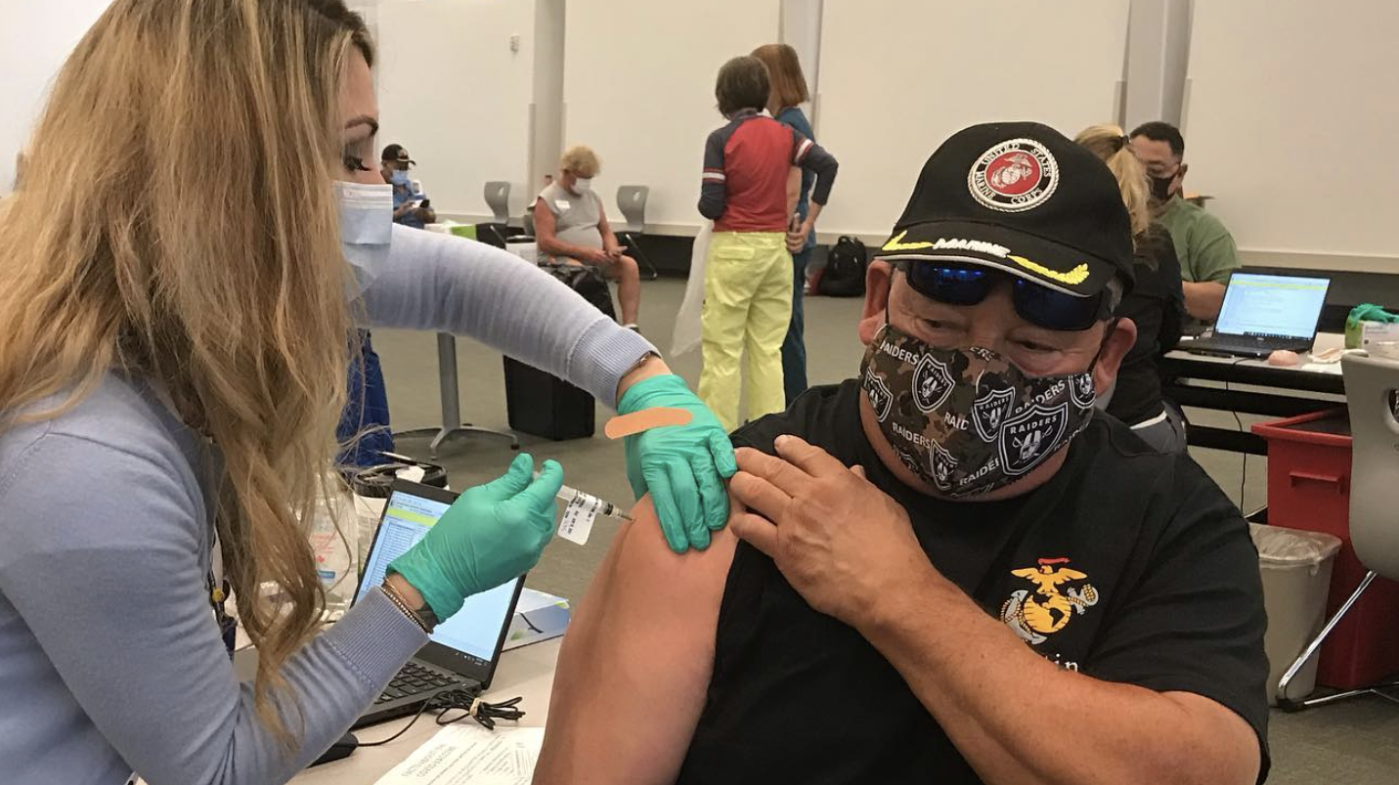
Respiratory illness season is approaching. Vaccines can help protect from flu, RSV (Respiratory Syncytial Virus), COVID-19, and pneumococcal pneumonia. These vaccines are available free of charge to Veterans receiving care at VA.
In a new series that highlights advancements in VA health care, VA researchers and clinicians are appearing on a Veteran-themed media platform—Wreaths Across America Radio—to tout their critical work.
Recently published findings from the VA Disrupted Care National Project [...]