To help decrease cancer deaths, VA is part of the White House Cancer Moonshot initiative, which aims to reduce cancer mortality by 50 percent in the next 25 years.
As one of the largest providers of oncology services in the U.S., VA cares for more than 450,000 Veterans with cancer and makes 43,000 new cancer diagnoses per year. In support of the initiative, multiple VA program offices are working to develop cutting-edge technologies and clinical practices that improve Veteran cancer care.
VA has made significant strides in preventive care, cancer screening, accessible treatment, and targeted cancer therapies.
VA approaches cancer care as a continuum that starts with cancer prevention and screening. With between one to two million Veterans at risk of developing lung cancer, VA’s tobacco cessation programs help reduce the biggest risk factor – smoking. Cancer screening is also critical because, in some cases, it can prevent cancer from developing entirely.
VA diagnoses cancer sooner through its enhanced screening capabilities, such as its award-winning lung cancer screening programs. VA also launched a pilot program to mail screening tests for colorectal cancer – the second deadliest cancer – to Veterans’ homes.
Air Force Veteran Brian Sturgill knows the euphoria of surviving cancer firsthand.
“When I was working at VA, I got a workup done for a GI (Gastrointestinal) bleed and a tumor was discovered,” Sturgill said. “It was metastatic lung cancer. At the time, the only option offered to me was chemo radiation, and I was told I was incurable. But thanks to a pulmonary doctor who wanted to do better by me, I had surgery, a small bowel resection and a lobectomy. Twelve years later, I’m still here.”
Sturgill is fortunate to be a lung cancer survivor. As the deadliest cancer, lung cancer causes 130,000 deaths per year and is more common among Veterans than the general population.
National Precision Oncology Program is part of Cancer Moonshot
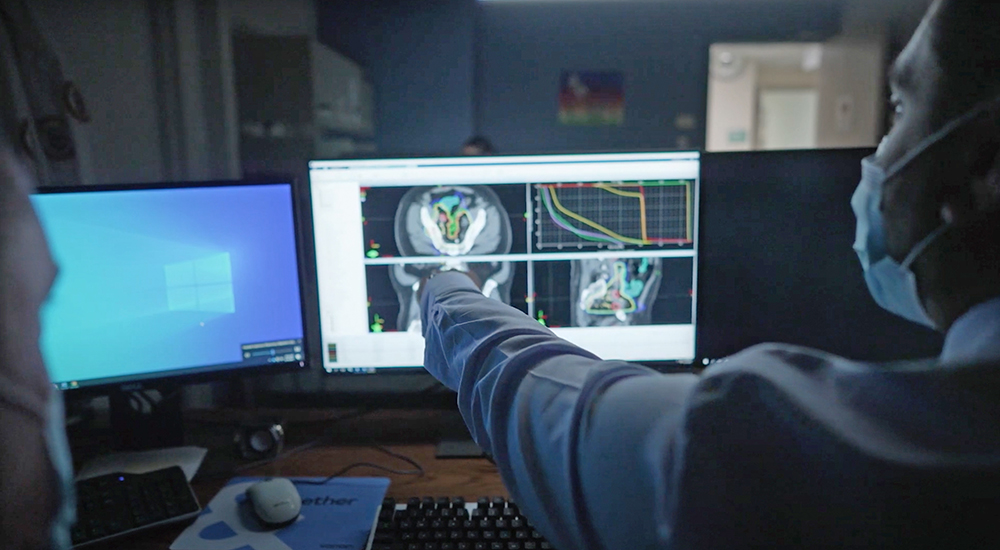
“Once diagnoses are made, it’s critical that cancer care reach Veterans,” said Dr. Michael Kelley, director of the VHA National Oncology Program. “This means treatment and care that is equitably distributed and accessible to everyone.
“Rural areas are generally underserved in terms of access to high quality care, particularly highly specialized care,” Kelley continued. “VA’s National TeleOncology service provides state-of-the-art sub-specialized cancer care to Veterans across the country. Nearly 60 percent of the Veterans seen through the service are rural.”
To provide the right cancer treatment at the right time, VA also launched the National Precision Oncology Program as part of Cancer Moonshot. This program gives Veterans access to pioneering genetic testing that helps physicians choose the most effective cancer treatments. Genetic testing has guided the care of 12,000 Veterans so far in 2022.
Other areas where VA is advancing the Cancer Moonshot initiative include addressing rare cancers (25 percent of VA cancer diagnoses), integrating clinical research with practice-based treatments and expanding access to cancer clinical trials.
It also includes translating VA data into care and knowledge and improving cross-agency collaboration to ensure cancer care advancements reach Veterans faster.
For more information, visit cancer.va.gov.
Topics in this story
More Stories
William Snow, senior program specialist at HUD, explains how the Point-in-Time Count provides valuable data on Veteran homelessness.
Gratitude is a light that shines through life’s ups and downs. Embrace gratitude this holiday season in just five minutes for this week's #LiveWholeHealth practice.
VICK, a wheelchair-cleaning kiosk, is transforming wheelchair sanitation in VA hospitals with UVC technology.