An Air Force Veteran’s life recently changed forever when doctors at two VA medical centers, almost 2,000 miles apart, worked together and used new, advanced technology to restore his health.
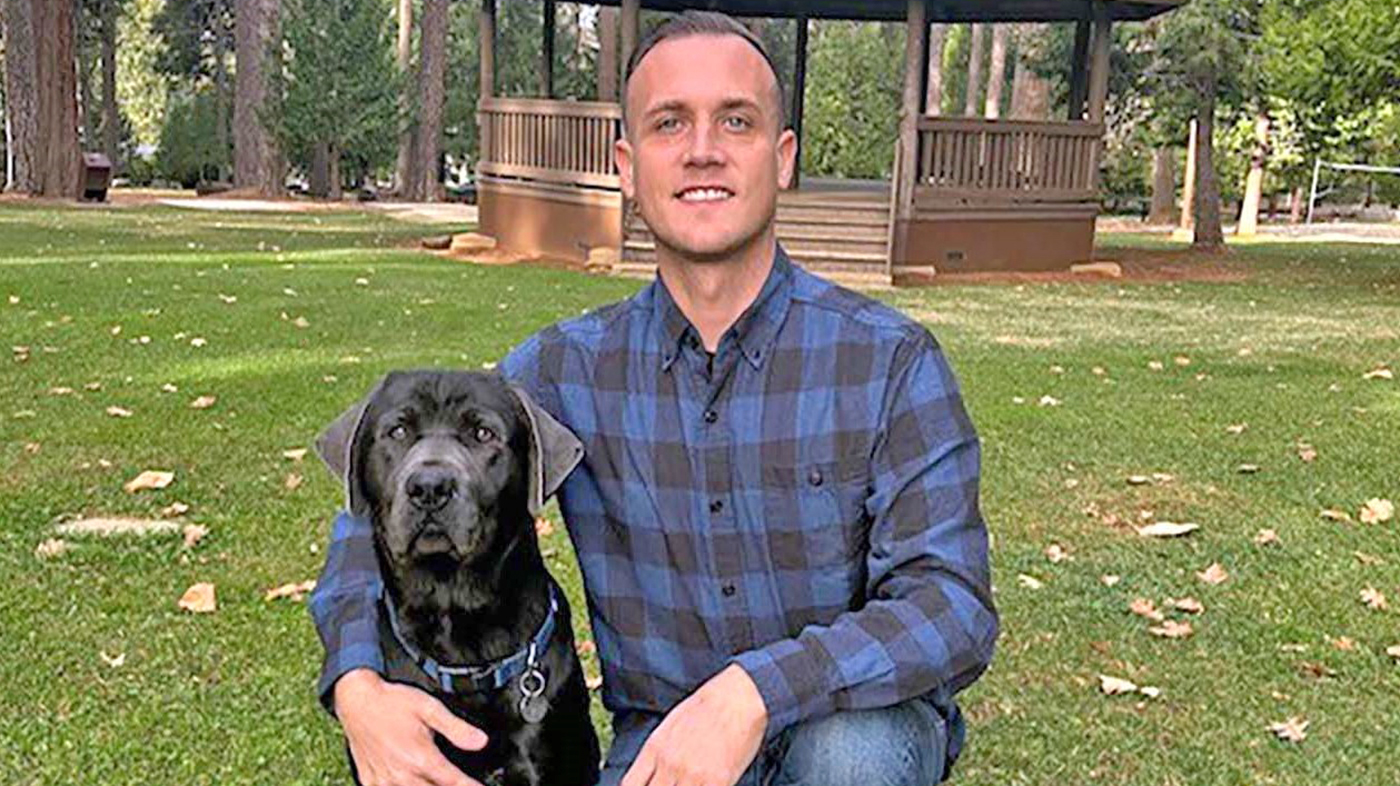
When Bryce De Witt (pictured above) got out of the Air Force in 2022, he was the picture of health. At 35-years-old and a father of four, he was physically fit, enjoyed CrossFit and hiking, and working his first post-military job as a firefighter and paramedic. Out of nowhere, he began experiencing low energy and a low heart rate.
“All of the sudden, I felt terrible. No energy and I passed out multiple times, so I was unable to work. With no history of heart issues in my family, I just knew there was something very wrong,” he said.
Impressed with VA doctor
For more than a year, De Witt sought help at community health care systems near his home in Foresthill, California. Exasperated, he turned to Mather VA in Sacramento. The staff there referred him to San Francisco VA and Electrophysiologist Liong Liem. Talking over Zoom, De Witt was immediately impressed with Liem and his team of experts.
“Within 24 hours of meeting Dr. Liem, I was scheduled for pacemaker insertion surgery. He took my concerns seriously and was in it with me every step of the way. He was determined to give me back my quality of life.”
After surgery, De Witt felt better, but still did not feel like his old self. His specialty care team at San Francisco VA suggested he consider a new technology available at Michael E. DeBakey VA in Houston, Texas.
Late last year, Houston VA offered Veterans with abnormally slow heart rates the new Aveir DR Leadless Pacemaker technology. This leadless system consists of two tiny pacemakers, each smaller than an AAA battery, that are inserted via a catheter in a large vein in the thigh. Without any incisions, the two devices are secured within the upper and lower chambers of the heart and work together to normalize the heart’s rhythm.
“Adding the second pacemaker makes all the difference,” said Electrophysiologist Dr. Hamid Afshar who, working with Cardiologist Dr. Irakli Giorgberidze, performed the procedure at Houston VA. “After reviewing Mr. De Witt’s history, we had a strong inclination that by upgrading the existing ventricular device to a dual chamber device we could help return his health to his normal baseline. This advanced, leadless technology is changing the pacing as we know it and can be an immediate game-changer for our Veterans.”
Doctors at Houston VA jumped at the chance to care for De Witt and collaborate with Liem and the San Francisco VA team.
Afshar is a professor of Medicine-Cardiology at Baylor College of Medicine and board certified in internal medicine, cardiovascular disease and clinical cardiac electrophysiology. “We are committed to working together to get the best results for our Veterans.”
Walking around the airport
In Houston, De Witt underwent the short 30-minute procedure. Straightaway, his two pacemaker devices began communicating through electrical pulses to ensure every heartbeat stayed in sync. De Witt was discharged from Houston VA the next day.
“I walked out of Houston VA and went straight to the airport to come home. I felt so good that I found myself walking around and around the airport. The VA doctors literally gave me my life back,” he said.
According to Giorgberidze, who is also director of Houston VA’s Electrophysiology Lab and an associate professor at Baylor College of Medicine, the dual pacemaker technology was a perfect fit for De Witt.
“With this new, advanced technology, there are no wires implanted in veins, no metal device under the skin and no surgical incision,” said Giorgberidze, who is board certified in cardiovascular diseases, clinical cardiac electrophysiology and internal medicine. “This means the potential for less risk, greater comfort and fewer post-procedure restrictions for Veterans. Our goal is to improve our Veterans’ quality of life and leadless pacemakers in both chambers of the heart are incredibly successful.”
Following his procedure in Houston, De Witt has fully resumed his physical activities and is now working as an emergency department technician and enrolled in nursing school.
“My plan is to ultimately work at VA,” he said. “VA has been the best health care I’ve ever received and I want to be a part of that.”
Topics in this story
More Stories
Ignoring challenging emotions can negatively impact our health. Breathe through worry, anger and sadness in 5 minutes with this week's #LiveWholeHealth practice.
Gulf War Illness committee provides advice to the VA Secretary. Meetings can be attended in person or virtually.
VA permanently housed 47,925 homeless Veterans in fiscal year 2024, exceeding its goals for the third year in a row.








WHAT A WONDER-FILLED STORY…NICE TO HEAR…SHARE….BUT…BUT…WHAT WILL THE VETERANS HEALTH ADMINISTRATION MEDICAL PROGRAM DO TO “FIX” THE BROKEN…FAILED…COMMUNITY CARE MEDICAL SYSTEM, THE FAILED FOREIGN MEDICAL PROGRAM REIMBURSEMENT PROGRAM, AND MOST OF ALL PROVIDE A REAL PAIN CARE PLUS PAIN DRUG THERAPY AND FAMILY EDUCATIONAL
PROGRAM?
WHY…WHY…DOES THE VA NOT DISCLOSE (IF THEY REFUSE TO INVESTIGATE AND PUBLISH THE RESULTS OF ANY
EVALUATION….PRE-IMPACT SURVEY THAT THEY HAVE RECEIVED OR NOT RECEIVED ….TO DATE????
WHAT TO DO ABOUT WHY THE VA PHARMACY BEEN ALLOWED TO TERMINATE ALL PAIN DRUGS…OR EVEN LIMIT THAT OF CIVILIAN PHARMACY PAIN DRUGS RX SUPPLY ?
WHY HAVE THE VA BEEN ALLOWED TO DENY PATIENTS PROPER DOCTOR PAIN PRESCRIPTIONS AND DIAGNOSIS…
TO IGNORE THE SWORN DOCTORS OATH TO DO NO HARM…?
WHY…AND HOW HAS THE VA ADMINISTRATION MEDICAL PROGRAM BEEN ALLOWED TO OVER-CONTROL AND LIMIT (BY AND OF OUR GOVERNMENT ) FOR CONTROL OVER THE CIVILIAN MEDICAL WORLD?
I felt proud to read this article. I have also had successful healing from skill decisions made by caring professionals at the VA health facility.