Robert Sullins, Jr., 63-year old Army Veteran, wears a left ventricular assist device (LVAD), which is a surgically implanted, battery-operated, mechanical pump. Used increasingly for end-stage heart failure patients, the pump helps his heart’s left ventricle—the organ’s main pumping chamber—pump blood to the rest of his body, prolonging and improving his life.
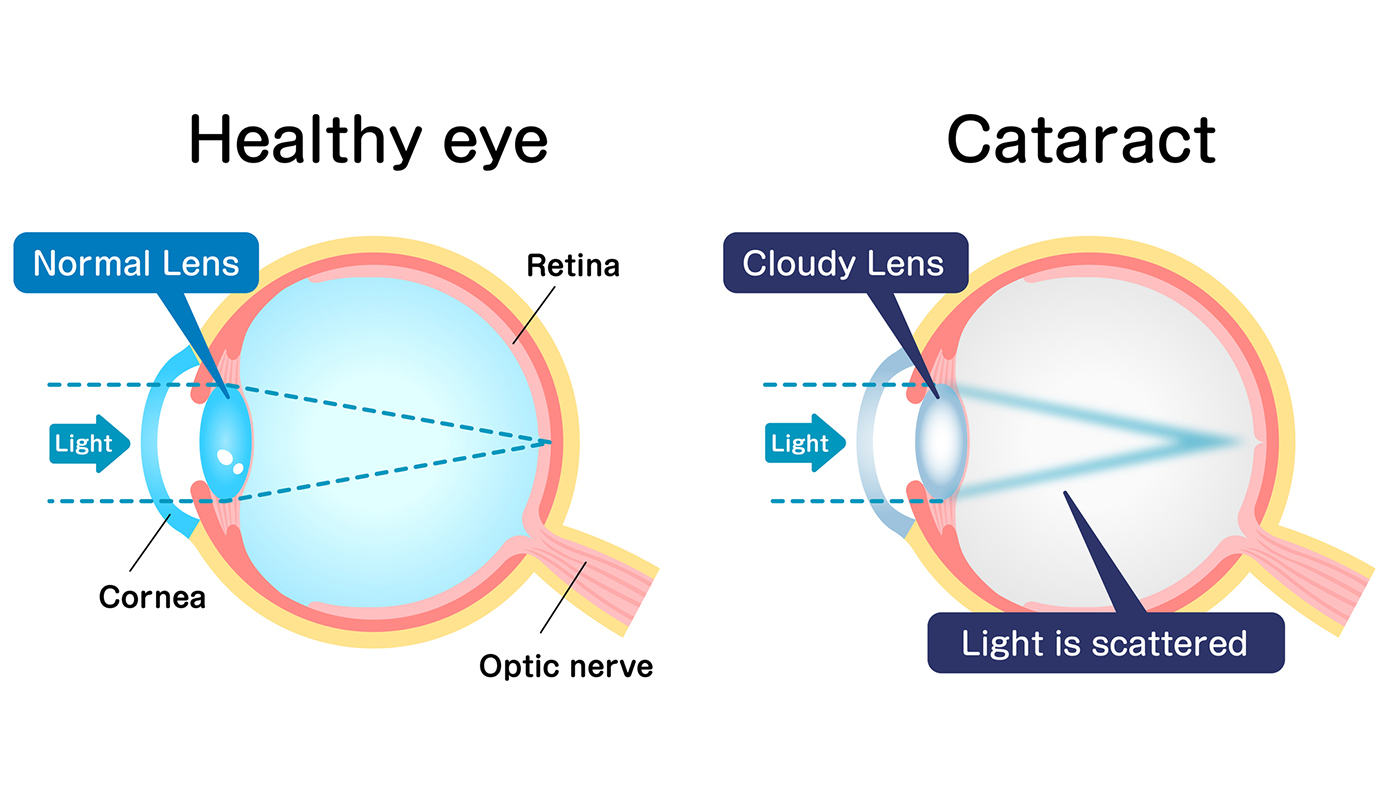
Although he’s lived with this life-saving device since 2021, the important role it plays in keeping him alive proved to be a challenge for clinicians when he needed cataract surgery. Because the technology is relatively new, there is little information or experience with patients wearing this device needing invasive surgical procedures. For this reason, when he approached an array of eye surgeons, there was general reluctance about conducting the procedure.
“I can never take it off. We have multiple battery packs so that it never runs out of power, and my wife is a certified caregiver for me as she has been taught how to change the batteries,” Sullins shared.
Team coordinates for surgery
Dr. Wuqaas Munir, chief of ophthalmology at Maryland VA and Sullins’ ophthalmologist, presented the case to the Peri-Operative Services director for evaluation. The director coordinated with a team of cardiologists at Baltimore VA and the University of Maryland, including a VA cardiology nurse practitioner who has extensive experience and training in LVAD technology and the LVAD cardiologist at the University of Maryland.
The company that manufactures the device was also contacted and a company representative agreed to be present during the procedure. With extensive communication between various clinicians at Baltimore VA and the University of Maryland Medical Center, they evaluated the safety of the procedure.
The Peri-Operative Services director who reviewed the records and discussed them with the cardiologists concluded that they could safely perform the surgery at the Baltimore VA with Sullins’s VA nurse practitioner and the LVAD company representative present in the operating room. Both are knowledgeable about the operation and functioning of the LVAD machine.
The surgery went well and Sullins is now scheduled for his second cataract surgery.
“We thought the LVAD heart device would pose a challenge,” said Munir. “With a lot of coordination, we were able to successfully complete the procedure using a local anesthetic.”
For Sullins, the surgery alleviated a lot of stress brought about by the increasing restrictions of diminishing vision. “I can see again and use my computer again,” he said. A second procedure will enable him to resume driving.
Topics in this story
More Stories
Bob Jesse Award celebrates the achievements of a VA employee and a team or department that exemplifies innovative practices within VA.
The Medical Foster Home program offers Veterans an alternative to nursing homes.
Watch the Under Secretary for Health and a panel of experts discuss VA Health Connect tele-emergency care.







There was no need for all the fuss. The cataract procedure is local and has no impact on heart function. M.M., O.D.