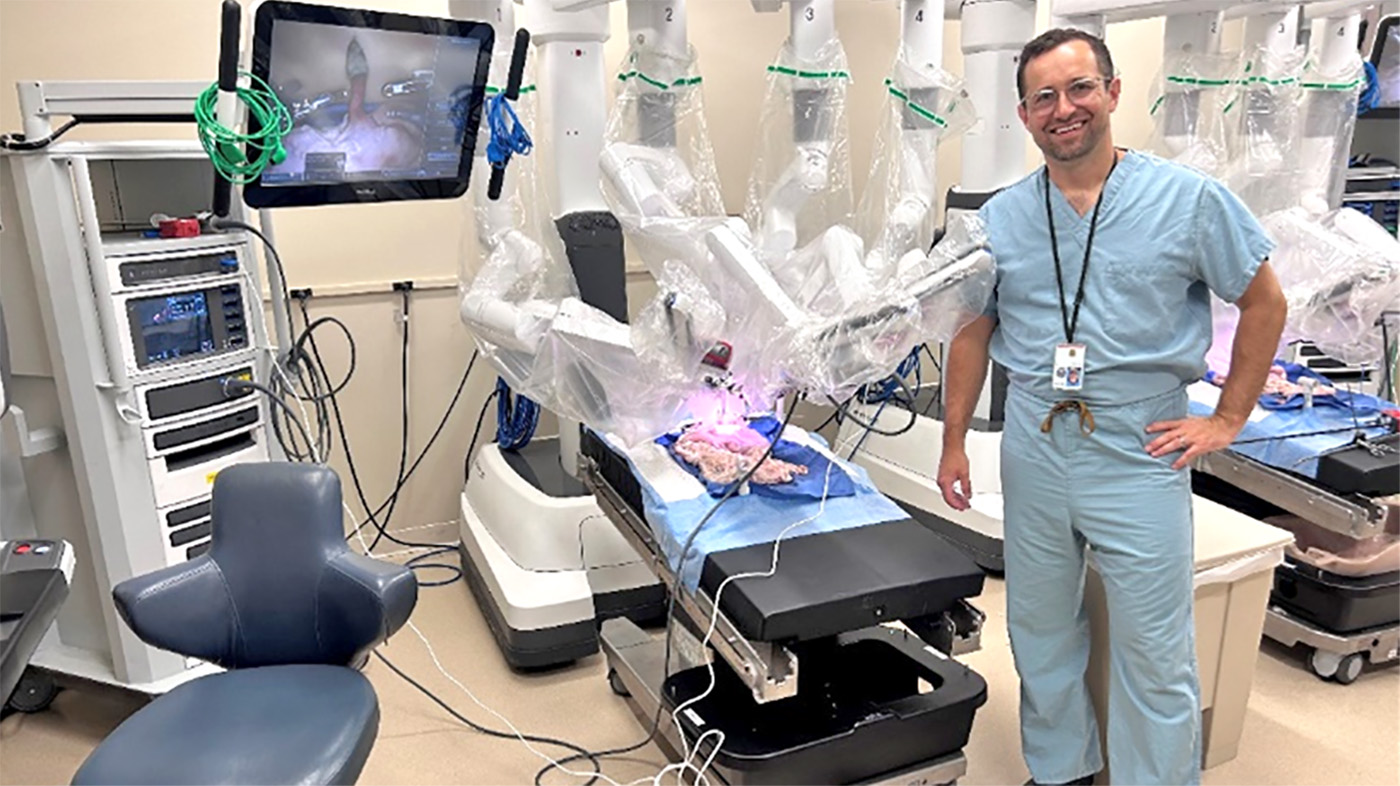
Physician assistant (PA) Matthew Vercauteren works at Pittsburgh VA but trains medical residents, attending surgeons and PAs from far and wide to use robotics during surgical procedures.
Robotic surgery is a minimally invasive surgical technique that uses robotic arms to perform procedures while a surgeon manipulates the arms from a console equipped with a viewing screen and controllers. PAs frequently serve as the primary surgical bedside assistant during these complex procedures and play a vital role in patient care and safety.
Robotic surgery is associated with decreased patient pain and recovery time compared to traditional procedures.
Vercauteren (pictured above) helped develop one of the nation’s largest robotic thoracic surgery training programs. Based on his expertise in robotic thoracic surgery, he was contracted by the Pittsburgh VA robotic thoracic surgery program and hired into a permanent position.
“I saw the excellent level of care of the VA staff.”
“At VA in 2012, I observed the commitment that all the physician assistants had to their patients and how they embraced the VA mission. While doing contract work at VA, I again saw the excellent level of care and dedication of the VA staff and I had a renewed sense of what it meant to work at VA. In 2020, at the onset of the pandemic, a thoracic surgery position opened up, and I jumped on the opportunity to bring my skills to VA and treat those that served our nation,” Vercauteren shared.
Vercauteren also champions robotic bronchoscopy, a technique to diagnose and treat lung cancer that had its VA debut in Pittsburgh. He also develops and provides robotic bronchoscopy training opportunities for residents, attending physicians and medical students, and he’s been invited to assist with robotic training sessions throughout VA while contributing to more than a dozen journal and book publications on the subject.
“Learning how to teach didn’t just come naturally. The first time I held a lab for residents and attending surgeons was nerve-wracking. However, with years of experience and having excellent mentors, I now truly love doing it. It reminded me of the feeling I had prior to playing the drums at my first live high school rock band show,” he said.
“A few trips to the hardware store and the model was created.”
In 2018, at the University of Pittsburgh Medical Center, Vercauteren was asked to develop a training model to perform a robotic-assisted surgical procedure used to treat Achalasia, a rare swallowing disorder.
“Never backing down from a challenge, I went to my garage and started to tinker. With the assistance hotrodder and Vietnam War veteran Frank Dempster, I was able to come up with a model that could be used to mimic many robotic procedures. A few trips to the hardware store and Uncle Frank’s garage… and the Heller myotomy 2.0 model was created,” he said.
Vercauteren continues to share his knowledge and to collaborate with experts to improve the health care provided to Veterans. “VA’s commitment to research, education and, above all, serving our Veterans, keeps me at VA,” he added.
Learn more about VA’s incorporation of new technologies and their impact on health care.
Topics in this story
More Stories
The Medical Foster Home program offers Veterans an alternative to nursing homes.
Watch the Under Secretary for Health and a panel of experts discuss VA Health Connect tele-emergency care.
The 2024 National Veteran Suicide Prevention Annual Report provides the foundation for VA’s suicide prevention programs and initiatives.






Great
It’s proof that the world has made advancements in surgery, yet as Africans, there are still some places where even laparoscopy is unavailable, and even open surgery is performed with outdated procedures that were phased out over 50 years ago.
This must be that “gubment” healthcare everyone’s been squealing about. Doc Larry’s comment should resonate though haha.
He isn’t teaching physicians to do surgery, he is teaching them to use the equipment much as a rep for the company would. In the world of surgery we have a saying: “see one, do one, teach one”. For your patient’s sake I hope seeing one is as far as he got.
The surgeon should have an eagle’s eye, a lion’s heart, and a lady’s hand