North Texas VA recently introduced a breakthrough in cancer treatment for Veteran patients with the unveiling of a new molecular imaging system. Better imaging in health care increases early detection and identification of diseases, improves patient outcomes, reduces costs and saves lives.
It gives clinicians a high-precision tool designed to spot cancer early and treat it accurately, helping Veterans on their path to recovery in ways previously thought impossible.
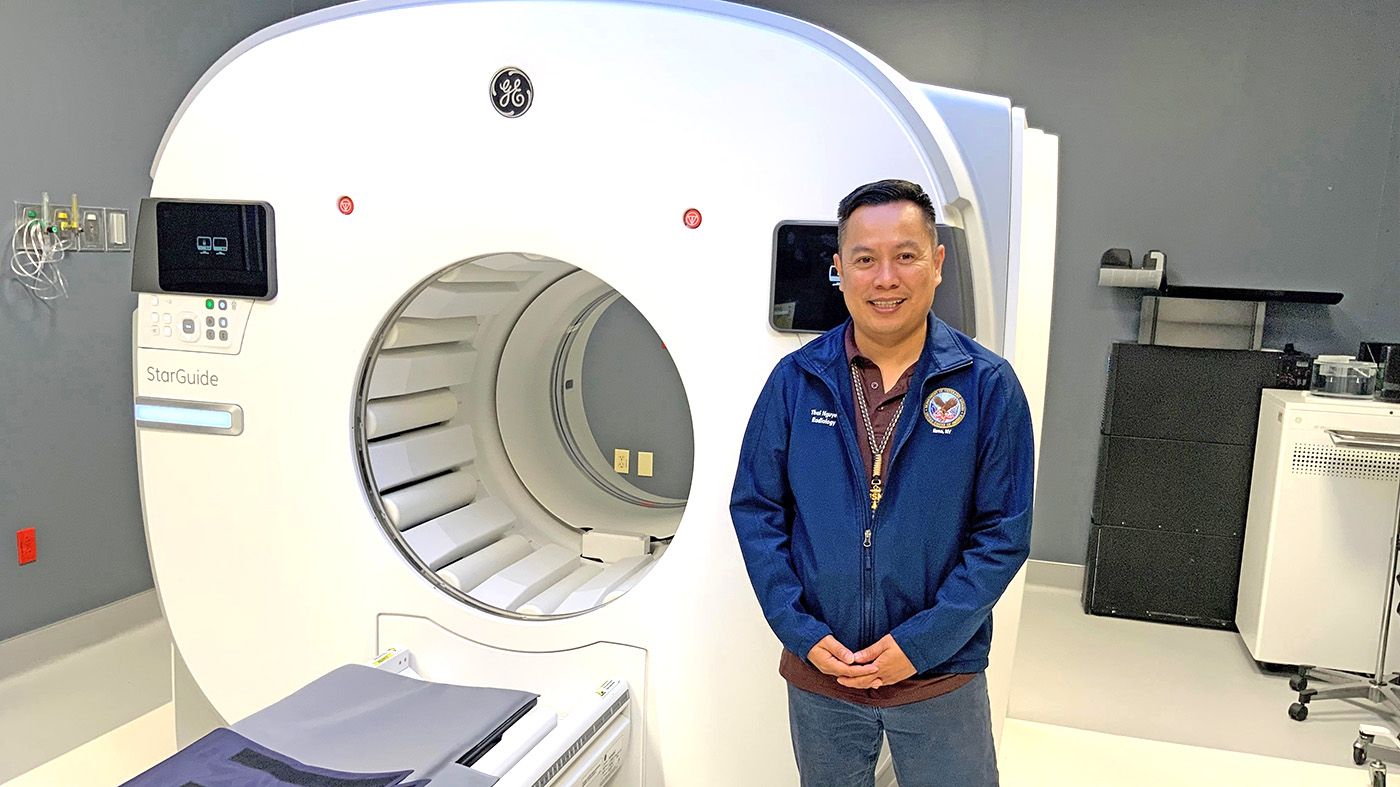
“This is not just a simple scan,” said Nuclear Medicine Technologist Thai Nguyen. “It’s a powerful tool that helps clinicians identify cancerous diseases earlier and treat them with greater accuracy.”
The system’s high-resolution images, faster scans and ability to generate a large amount of data help physicians see clear images that detect diseases at an earlier stage. The cutting-edge system goes beyond traditional scanning. It’s a pivotal shift in how cancer is detected and addressed.
A “GPS” for cancer
Traditional treatments, such as chemotherapy, often affect all cells in the body which can lead to a range of side effects. This technology takes a different approach. It directs treatment to diseased cells, minimizing harm to surrounding healthy tissue.
This precision allows the medication to act like a cancer GPS, reaching only the cancer cells and sparing nearby tissues.
This technology offers a significant advantage for patients. With fewer side effects and a highly targeted approach, it delivers a new standard of cancer care that aligns with the unique needs of our Veteran patients.
The molecular imaging system’s detectors are positioned about two inches from the patient’s body, allowing for ultra-detailed 3D resolution. The detectors rotate 360 degrees around the patient scanning from all angles for a greater view of the targeted area.
It also marks a major milestone for VA’s dedication to serving Veterans with the best medical technology available. It stands as a “gold standard” for cancer care within the VA system, providing a vital resource for Veterans in North Texas, Oklahoma and beyond who are fighting cancer.
Future of cancer treatment at VA
“This technology’s impact reaches far beyond oncology, supporting areas like cardiology, neurology and bone procedures, positioning VA as a leader in the medical field and a standard-setter for cancer care,” said North Texas VA nuclear medicine chief Dr. Irfan Farukhi.
For Veterans and their families, the introduction of this new technology isn’t just a new piece of equipment. It’s a sign of hope and a commitment to delivering the best possible care and improving the lives of those who have served.
Topics in this story
More Stories
The Medical Foster Home program offers Veterans an alternative to nursing homes.
Watch the Under Secretary for Health and a panel of experts discuss VA Health Connect tele-emergency care.
The 2024 National Veteran Suicide Prevention Annual Report provides the foundation for VA’s suicide prevention programs and initiatives.







For some of us, we dont need the article dumbed down.
This is a CT scanner from what I can tell by the image. It has its pros and
cons in types of imaging. Like soft body Lipomas that can trick it. Its
harder to find a liposarcoma with a CT scan till its too late. Just comes
up as a gray blob.
Ive been fighting tumor imaging issue all year long with a now massive
lipoma that cant be quite figured out. Today I do a pre post IV contrast
MRI in a hope to visualize a possible pulmonary nodule. Taken 3 months
to find someone who would do it. As lungs and MRIs are a big issue.
You say lung, they dont do MRIs of them.
When you deal with difficult locations, and difficult formats – VISN 17
tends to break down. Turns out this tumor has been there in 2018 and
the first lab tech missed it. Not the Thorasic surgeon later. Because it
wraps around the back of the lung and spread out like a pancake. He
showed it to me in his lab.
There are so many possible cancers, and early detection is still not there
for so many of them. Time is critical.
I would rather read technical data about your method than bragging that
you have it. Wasnt offered to me? Might be after today. Only this damn
MRI is 1.5T and really I should be in a 3T to 5T for greater accuracy.
Multiphasic MRI is a confusing term, and it shouldnt be. Terminology stops
so many things cold because VA trips up over “words”. Its the law, and so the
law is up for grabs when things get dicey. People die over words,
misunderstandings. Long protracted events that didnt need be.
I hope to address this to the VA Research Advisory Committee meeting
in Houston on November 20, 21st 2024 to discuss legal loopholes in
veterans imaging. How specialty care or clinics are needed to assist these
programs with medical oddities not seen in the general population. My
so called Toxic Exposure Pathology Center that could expedite tissue
biopsy and identification early on.
There is what VA is doing, and there is what we vets are living. In that grey
area is a 20 year wait time between identification and application. When
VA stalls and delays potential avenues with legal mumbo jumbo.
I need the hows and whys now, and way to fix that if its too slow. It has been.
What a great machine for people getting cancer. Not just Veterans but ALL PEOPLE.
This cancer finding equipment, is it available to vets in other locations, such as San Diego??