Increasing numbers of women Veterans of childbearing age are enrolling in VA health care. Consequently, information on optimizing pregnancy outcomes is important for women Veterans, their families, and their providers. Since 1981, the surgeon general has advocated that women who are pregnant or trying to conceive not drink any alcohol. This recommendation, which was reissued in 2005, is built on a strong foundation of scientific evidence that alcohol exposure during pregnancy is harmful to the developing fetus and may result in fetal alcohol spectrum disorders (FASD).
As we continue to observe Alcohol Awareness Month during April, it is an appropriate time to learn more about FASD and its potential impact on women Veterans and others.
FASD is an umbrella term that encompasses a range of adverse outcomes related to fetal alcohol exposure. At the most severe end of the spectrum are children with fetal alcohol syndrome (FAS), a condition characterized by facial anomalies, growth deficiency and brain abnormalities. The facial features include a thin upper lip, a shortened distance between the inner and outer corners of the eye, and smoothing of the groove underneath the nose. Height, weight and head circumference are frequently reduced. Brain abnormalities result in intellectual disability, behavioral problems, and social challenges. Attention deficit hyperactivity disorder is common, and many affected children struggle with learning, memory, planning, impulse control and arithmetic.
Most children with FASD do not have the full FAS. Alcohol is harmful to the developing brain throughout pregnancy, and the characteristic facial features of FAS result from alcohol exposure during a very narrow time window—approximately day 17 of pregnancy. Children exposed to alcohol at other times during pregnancy lack the visible birth defects of FAS, yet may still experience the same intellectual, behavioral, and social challenges as children with FAS. The absence of facial abnormalities makes diagnosis of these children more difficult.
FASD is the most common preventable cause of intellectual disability in the United States. FASD experts have examined large numbers of first-grade children in communities across the United States, Europe and Africa. From these community-based studies, the prevalence of FASD in the U.S. has been estimated to be between 2 and 5 percent, a rate equal to or greater than that for autism spectrum disorder. In some communities in the wine-growing region of South Africa, the prevalence of FASD exceeds 10 percent.
Fetal alcohol exposure is sufficient to cause FASD; however, additional factors influence the severity of FASD. Perhaps the most important of these factors is maternal nutrition. Children heavily exposed to alcohol during pregnancy are more likely to have FASD if their mother was malnourished. Outcomes after heavy alcohol exposure are improved in children whose mothers take prenatal vitamin supplements. The effects of prenatal alcohol exposure may be worsened by smoking and exposure to other drugs. Animal studies suggest that cannabinoids, active ingredients of marijuana, may worsen birth defects caused by alcohol. The genetics of the mother and the child are also important. Non-identical (fraternal) twins are exposed to the same levels of alcohol during pregnancy, yet only one may be born with FASD. In contrast, if one identical twin has FASD, the other is more likely to also have FASD. Fraternal twins share half of the same genes, and identical twins have identical genes. Hence, it is likely that some genes are protective and others increase the risk for FASD. Experiences of early childhood may also improve or worsen outcomes after prenatal alcohol exposure. Children who grow up in loving homes and enriched environments are more likely to have better outcomes after prenatal alcohol exposure than those who are neglected and have few stimulating activities.
There are challenges and opportunities in the prevention of FASD. Alcohol can harm the fetus even prior to pregnancy recognition. Binge drinking produces high peak blood alcohol concentrations, both in the mother and in the fetus, and high blood alcohol concentrations are especially damaging early in pregnancy. Day 17 of pregnancy represents a particularly vulnerable period for alcohol exposure and is just two days after the first missed menstrual period—a time when many women are unaware of their pregnancy. A second concern is that approximately half of all pregnancies are unplanned. Many women of childbearing age have sex without contraception, and alcohol use increases this practice. These risks are compounded by a rising rate of binge drinking in women in their teens and 20s. Together, the high rate of unplanned pregnancies and fetal vulnerability to alcohol prior to pregnancy recognition pose a unique risk for FASD that is heightened in Veterans with alcohol use disorder. Sexually active women may choose to reduce these risks through increased contraceptive use and reduced binge drinking, especially prior to pregnancy recognition.
Is any level of alcohol exposure safe for the developing fetus? Research studies in cells, animals and humans have not established a safe level of alcohol exposure. In fact, exposure of rat brain cells to concentrations of alcohol attained in the blood after just one drink interferes with the function of a molecule that is required for normal brain development. Some, but not all, human studies demonstrate intellectual and behavioral effects in children after mild to moderate drinking during pregnancy. The inability to demonstrate a safe level of alcohol exposure for the developing fetus reinforces the surgeon general’s warning to avoid alcohol use altogether while pregnant or trying to conceive. Sexually active women who are not trying to conceive and who choose not to use contraceptives may avoid binge drinking or not drink at all. Women who have had a few drinks before pregnancy recognition need not panic that they have harmed their unborn child. Outcomes of these pregnancies are usually good, especially if further fetal alcohol exposure is avoided and nutrition and general health are well-maintained.
About the author: Michael E. Charness, M.D., is chief of staff at the VA Boston Healthcare System. He is also a professor of neurology and associate dean at Harvard Medical School and at Boston University School of Medicine. Widely known for his research on the health impacts of alcohol use, Dr. Charness has been with VA since 1989.
Topics in this story
More Stories
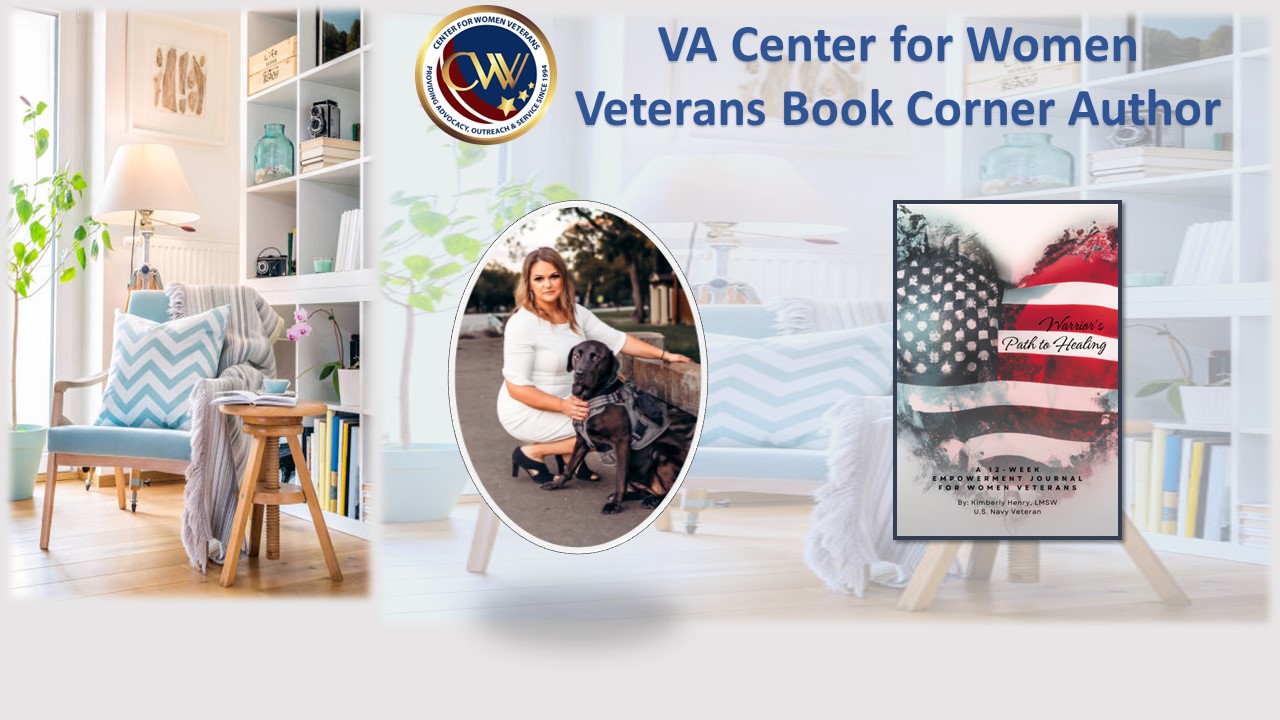
This month's Center for Women Veterans Book Corner author is Navy Veteran Kimberly Henry, who served as a Cryptologic Technician and Sexual Assault Victim Advocate from 2009-2019. She created "Warrior's Path to Healing: A 12-Week Empowerment Journal for Women Veterans."
Thinking about building a family or exploring fertility treatments? VA can support you with a wide range of services.
Report examines the input of over 7,000 women Veterans: They are happier with VA health care than ever before.