For the latest on VA’s response and inspiring stories of service to Veterans impacted by the hurricanes, read more on the blog. For those impacted by Hurricane Harvey, click here. For information on Hurricane Irma, click here.
The pills had been right there on the kitchen counter. And then, they were gone.
In the wake of Hurricane Harvey, as flood waters rose quickly, one Army Veteran worked to help his terminally ill wife out of their Houston home. He had already freed his truck from the flooding, and they were all set to leave, but then he realized the waters must have swept his pills right off the counter.
The Veteran needed the antibiotics for an infected ulcer on his left foot; all this time in the flood water wasn’t helping. He grabbed a trash bag and wrapped it around his leg, but the splashing soon pushed it off.
“He’s panicked, because he’s in these waist-high waters, and he has this open wound that’s soaking in these dirty waters,” said Dr. Leonie Heyworth, VA’s acting national telehealth advisor for primary care. “He already lost his left big toe last year, so this baby toe on his left foot would be the second toe he would lose if the infection progressed.”
In the immediate aftermath of Harvey, as Houston faced catastrophic flooding, the VA activated its emergency response system, providing shelter, food, medicine and other services to Veterans in need.
In one change this summer, the VA also included telehealth as part of this emergency response system. The Office of Connected Care’s mobile and telehealth programs, in coordination with the Houston VA and VA’s regional network, quickly organized telehealth capabilities to assist Veterans at two mega-shelters and four community based outpatient clinics. Remote clinicians used VA Video Connect and other video technologies to hold virtual health care appointments with Veterans.
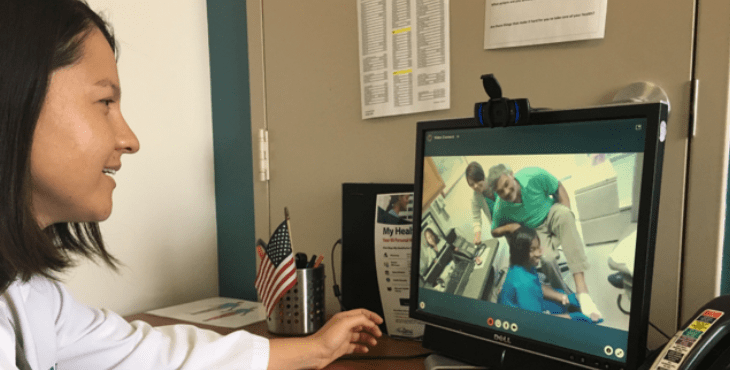
And so, a week after rescuing his wife from their home, the Veteran was able to sit across from a webcam and consult a VA clinician in San Diego about his infected ulcer.
“He’s imploring on me to please give him some good and strong antibiotics, because he really can’t afford to lose another toe on his left foot,” said Heyworth, who conducted the appointment. “He needs to be able to be strong to take care of his wife, who is undergoing chemotherapy for advanced breast cancer.”
The nurse shifted the exam camera down, and Heyworth evaluated his toe. It was bright, angry red, with patches of black. The open wound was weeping. Concerned, she prescribed a new course of antibiotics.
And as she sat at her desk, more than a thousand miles away, Heyworth was struck by their ability to connect on a very human level through mobile technologies. The Veteran opened up about his struggle, at one point placing his head in his hands and crying. “I felt very much like I was there with him in the room,” Heyworth said.
At the end of the appointment, he handed his cell phone to the nurse, put his arm around the desktop monitor and posed for a photo with Heyworth. He joked that he’d seen enough water to last a lifetime, and wondered if they could send some to California. “Stop by next time you’re in Texas,” he told her, before limping out of the room.
“I think it really spoke to me,” Heyworth said, “that you can create that patient-doctor relationship virtually, and mobilize resources on the ground that will help people.”
Later that day, just before the clinic closed, one of the nurses messaged Heyworth that another Veteran had come into the waiting room.
His house was on higher ground, so they had been able to handle the rising waters. But he was now overdue to see a clinician about the results of a urine culture. He was using a catheter to urinate, and fearful that he may run out of resources during the flooding, he had limited what he was drinking and rationed how often he was using his catheters.
He began to feel ill, so when he learned the clinics were seeing people again, he headed in.
Right away, Heyworth could see something was wrong, as a very rapid heart rate popped up on her screen and his temperature came in at 102. “I’m worried,” Heyworth remembered, “because this patient could have an infection from his urine that’s tracking into his kidneys and into his blood stream.”
She reviewed the results of his urine culture and identified that his infection was resistant to the antibiotics he’d been taking. She directed him to the Houston VA Medical Center’s emergency room, where he was able to receive IV fluids and specialized antibiotics.
“The bottom line is that telehealth is meeting Veterans where they are,” Heyworth said. “We are making things flexible and convenient for them.”
One week later, the Veteran Heyworth connected with about his foot was able to walk again on his toe. The redness and swelling had subsided significantly.
“To be able to very quickly get in there, and quickly see patients, was incredibly gratifying,” Heyworth said. “Because it made me feel like I was there. It made me feel like I was contributing to the needs of these Veterans at a very vulnerable time in their life. And I will certainly always remember that. They will always feel like my patients. I will always remember their stories.”

Topics in this story
More Stories
Daughter and son-in-law find a diary of her father's life as a prisoner of war written on toilet paper.
VA announces positive Veteran satisfaction feedback on telehealth services, including video visits, in the first half of fiscal 2025.
The VA Bay Pines stand down relies on volunteers to connect Veterans facing homelessness with the resources they need.