In the two-plus years that the Houston VA’s Breast Imaging Center has been in operation, more than 14,000 breast exams have been performed and the Breast Imaging Center has become a model of care across the nation’s VAs for Women Veterans.
“We started our program from the ground up and have molded it into a quality program that is comparable to some of the top-notch facilities in Houston,” said Dr. Mahdieh Parizi, chief of the Breast Imaging Center, whose sub-specialty is breast radiology. “Our goal was to set up a very elite, high-quality practice that can meet the needs of our Veterans and be a shining star in the Houston community and beyond.”
This is precisely what the facility has accomplished. The center boasts two 3-D mammography machines, each equipped with the latest Smart-Curve technology and high-resolution detectors.
Smart-Curve refers to the paddles used during a mammogram which allows for a more comfortable exam. High-resolution, 3D detectors help discover cancers much earlier, which is a key to better prognosis. In fact, very few practices and facilities in Houston have the smart-curve technology and the high-resolution software.
New technology: Radiofrequency emitting tags tumors, cancer
Another new and cutting-edge technology that will be implemented by the Breast Imaging Center is the use of radiofrequency emitting tags to localize tumors for the surgery team. This new technology will make it more efficient and convenient for the patients to have localization of the tumors without having to be stressed about the use of a wire (the most common technology in place).
Additionally, this new technology allows for a more flexible and patient friendly timing between when the tag is placed and when the patient has excision of the tagged tumor, a factor that the patients greatly appreciate.
“We try to remove the anxiety from getting a breast exam,” Parizi said. “The majority of our patients get their results face-to-face before leaving the center. If we see an abnormality that needs a biopsy, we try to perform the biopsy before the patient leaves. In the private world, most patients go home and wait for a letter with their results. Here, we do everything the same day. They go home knowing what their results are and that alleviates a lot of anxiety.”
“I’m just so grateful that I have this facility.”
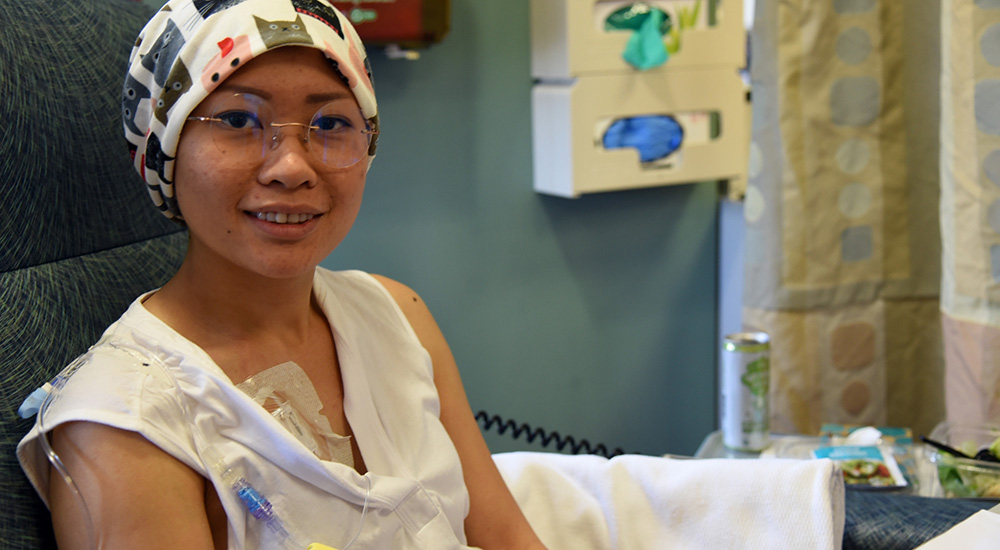
Army Veteran Kim Pham, 30, felt anxiety and depression when Parizi found cancer during a breast exam. Her cancer was a hair away from being stage-4 when treatment began. Pham (pictured above) has no family history of cancer.
“I felt like I had been punched into space,” Pham said. “Everything I knew was just completely shattered. It was the sensation of your life being turned upside down.”

Dr. Mahdieh Parizi, chief of the Breast Imaging Center, adjusts a mammography machine prior to a patient visit.
Parizi still calls Pham to check in on her to make sure she is doing well and in good spirits.
“I’m just so grateful that I have this facility,” Pham said. “I’m blown away by how fortunate I am. Everything lined up just right because I could be in a really bad situation right now.”
Top programs have three things in common and Houston VAMC has them all: The physician who interprets the mammograms is sub-specialized in breast radiology; use of 3-D mammography; and hires the most experienced technologists. This center checks each box. Its technologists have between 15-25 years of work experience.
“We brought all of these quality parameters together and we were able to create this amazing program, which became accredited with the American College of Radiology, and has passed annual FDA inspections two years in a row with perfect scores,” Parizi said. “Our next step is to become a Center of Excellence in breast imaging. Currently, the VA has 68 breast imaging programs and only one center of excellence (Phoenix). We hope to become the second.”
So, when should women Veterans get a screening mammogram to check for breast cancer?
Recommend screening mammogram once annually beginning at age 40
Currently, there are differing recommendations regarding screening mammography. However, Parizi points out that The American College of Radiology, the American College of Surgeons, and the Society of Breast Imaging—breast experts who are most knowledgeable about breast cancer and diagnosing it—recommend to get a screening mammogram once annually, beginning at 40 years old (even when a patient does not have a family history of breast cancer).
“The science repeatedly demonstrates that we save the most lives when we screen annually starting at age 40,” she said. “Up to 75% of breast cancers occur in women with no family history of breast cancer. The biggest risk factor is gender: simply being a woman.”
The Breast Imaging Center hosts a breast cancer support group for women who are currently going through breast cancer treatment or are survivors. This is unique to the Michael E. DeBakey VA Medical Center as many programs, including non-VA practices, do not have this type of holistic approach to the patient.
Todd Goodman is a public affairs specialist with the Houston VA Medical Center.
Topics in this story
More Stories
Watch the Under Secretary for Health and a panel of experts discuss VA Health Connect tele-emergency care.
The 2024 National Veteran Suicide Prevention Annual Report provides the foundation for VA’s suicide prevention programs and initiatives.
Theranostics is a specialized field of nuclear medicine that uses a two-pronged approach to diagnose and treat cancer.