The VA Phoenix Medical Center launched a new telehealth physical therapy (PT) clinic as part of Veterans’ post-op care plans after total knee replacements. The innovation empowers Veterans to begin VA outpatient PT at home within a week of surgery, improving Veterans’ experience of care.
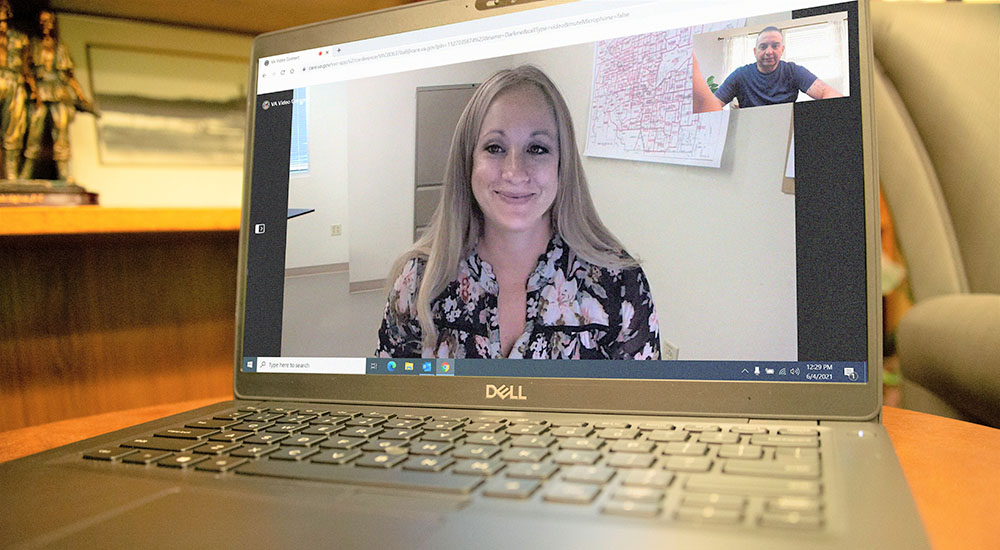
“Timely access to physical therapy is so important to get Veterans moving in a healthy pattern because sometimes, after surgery, we’re hesitant to move or we’re nervous,” said Christina Crawford, telehealth coordinator (pictured above). “Also, it can help to prevent tightness (known as contracture) in the knee, therefore improving the mobility of the knee.”
Hospital performs average of 35 total knee replacements a month
Phoenix VA performs an average of 35 total knee replacements a month. Crawford, a board-certified clinical specialist in geriatric physical therapy, noticed many of these Veterans were not starting outpatient PT within the recommended 21 days post-surgery.
“Once a Veteran gets home, they find they have barriers they didn’t even think of, such as driving a car,” she said. “Transportation is a major challenge to access to care.”
Crawford’s initiative was inspired by and developed as part of her engagement in the VA Geriatric Scholars Program, a national workforce development program.
It trains primary care providers in geriatric medicine and teaches fundamental skills in quality improvement based on the IHI Model for Improvement and Plan, Do, Study Act (PDSA) cycles.
VA Geriatric Scholars Program inspired changes
“After I attended the program, I came to the team and said, ‘Let’s break this down,’” she added. “We looked at the continuum of care from the moment we have the patient. That’s when we started implementing small changes.”
For her project, Crawford tapped into her experience as the VA Phoenix Medical Center’s point of contact for the enterprise-wide Rural Veterans TeleRehabilitation Initiative. Funded by the VA Office of Rural Health, the initiative empowers rural Veterans to access the care they need at home using VA Video Connect.
“One of the fantastic things VA does is address barriers to care in rural settings,” she said.
The aim of the team’s project was to improve access to outpatient PT within 21 days of surgery.
Improvement initiatives included four PDSA cycles:
- Creating a post-op PT telehealth clinic
- Educating providers and patients about telehealth PT
- Changing the referral process to PT post-op
- Providing postcards in the folder issued to Veterans at hospital discharge with PT clinic walk-in hours for quick service post-surgery
Patient-centered approach… it’s about the whole team
One of the first tasks was to educate and inform patients and providers about the new clinic. “Education and information were not just about the patient,” Crawford said. “It was about the whole team, making sure everyone was in on this collaborative approach focused on the Veteran experience.”
Patient education starts before surgery. “One of the great things at the Phoenix VA is we have a pre-operative class,” she said. “Before Veterans have surgery, they go to the class to learn about what to expect.” Working together with the orthopedic nurses who lead the class, the team added new information to the presentation to inform Veterans about telehealth PT.
Proactive outreach… you’re not alone
After the pre-op class, PTs proactively telephone Veterans to address any questions about telehealth rehabilitation. If interested, Veterans are scheduled for a telehealth PT visit one week from surgery.
Patient education occurs again the day of surgery. At Phoenix VA, PTs ensure Veterans are up and walking the day of their operation. Dr. Crawford helped this team learn the language of telehealth to establish a seamless transition from inpatient to outpatient care using VA Video Connect.
35 physical therapists on staff – “We’re ready to go.”
At the onset of the pandemic, elective surgeries at Phoenix VA were significantly reduced.
“We have 35 physical therapists on staff right now and all of them can do telehealth,” she said. “A year ago, there were only five therapists doing telehealth, at the most. There was definitely a learning curve, but they leaned in. The commitment of the PT team is fantastic. Currently, we are seeing an increase in patients electing to have total knee replacements, and we’re ready to go.”
Learn more about the VA Office of Rural Health’s Rural Veterans TeleRehabilitation Initiative – YouTube.
Maureen Jerrett is a communications contractor for the VA Geriatric Scholars Program.
Topics in this story
More Stories
Study underscores important role COVID vaccination can have in protecting Veterans from infection and reducing long-term health consequences
Columbia VA’s robotic surgery teams completed their 800th robotic surgery and are on schedule to hit 1,000 by the end of the year.
In a decentralized clinical trial, Veterans can participate from their own homes or local VA instead of having to travel to a research site.