VA Sierra Nevada Health Care System is proud to partner with a team of our pharmacists to encourage Veterans and their families to incorporate free Opioid Overdose Rescue kits into every household first aid and emergency kit.
Dr. Melanie Ginzburg has been leading efforts throughout northern Nevada and northeastern California. Joining her are Drs. Chanese Hampton and Carla Figura.
Ginzburg (pictured above) is an academic detailing/pain pharmacist, Hampton a substance use disorder pharmacist and Figura a pain pharmacist.
This team of pharmacists have been on the forefront of the VA OEND (Opioid Overdose Education and Naloxone Distribution) Program and they’re eager to educate Veterans and their families on the importance of keeping overdose rescue kits easily accessible.
“If every household had a rescue kit, lives can absolutely be saved”
“When we talk about safety, usually we think of common hazards in our homes,” explained Ginzburg. “But, sadly, more families nationally are experiencing loss of a loved one who overdosed on prescription or illegal drugs, often accidentally. If every household had an Opioid Overdose Rescue kit, lives can absolutely be saved. It is no different than keeping band-aids on hand. You may never need them but, if you do, they are there for easy, quick access.”
The National Center for Health Statistics at the Centers for Disease Control and Prevention uses the CDC Wonder website to track deaths involving many of the more commonly used drugs. According to CDC Wonder, in 2019, over 70% of drug overdose deaths involved an opioid.
Opioids are substances that work in the nervous system of the body or in specific receptors in the brain to reduce the intensity of pain. The most common drugs involved in prescription opioid overdose deaths include: Methadone, Oxycodone (such as OxyContin), and Hydrocodone (such as Vicodin).
Ginzburg: Keep a kit on-hand for anyone at risk of overdose
But heroin and synthetic opioids, like fentanyl, have seen a 6x increase in usage since 1999. Recently, Washoe County district attorney Chris Hicks stated that his “biggest concern throughout Nevada and the country is the frightening increase in our communities of methamphetamines, which include the deadly ingredient fentanyl.”
Reno VA and community partners have been working for years to address Veteran pain holistically instead of masking symptoms with drugs. But street drugs are easily accessible, affordable and their use is exponentially on the rise by people of all ages.
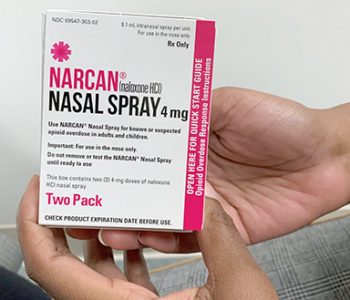
The Opioid Overdose Rescue kits include a Naloxone nasal spray. They’re free-of-charge at VA even if a Veteran has VA co-pays. Ginzburg urges Veterans to request and keep a kit on-hand for anyone they care about who is believed to be at risk of overdose.
“We want Veterans to know these kits do not have to be for themselves but also for those they love. Safety is paramount and sharing a new solution to save lives is rewarding.”
Anyone can purchase Naloxone sprays at their local pharmacy without a prescription. The kits are small enough to easily include in every first aid kit for your home and vehicle.
Most medical centers require a prescription for free kits
There are some VA medical centers that have policies in place for Veterans to be able to request naloxone from their pharmacy without a prescription from their primary care provider.
However, the majority of VA facilities require a prescription to be written by the Veteran’s provider. It can be from primary care, mental health, pharmacist, etc.
Veterans do not have to be using opioids to request a naloxone kit. There are no restrictions on who can have one.
For more video and brochure information, visit the VA Pharmacy Benefits Management Services page at: Academic Detailing Services – Opioid Overdose Education & Naloxone Distribution (OEND) – Pharmacy Benefits Management Services (va.gov).
Check out this OEND quick reference fact sheet.
Glenna E. Smith is the public affairs officer for the VA Sierra Nevada Health Care System.
Topics in this story
More Stories
Watch the Under Secretary for Health and a panel of experts discuss VA Health Connect tele-emergency care.
The 2024 National Veteran Suicide Prevention Annual Report provides the foundation for VA’s suicide prevention programs and initiatives.
Theranostics is a specialized field of nuclear medicine that uses a two-pronged approach to diagnose and treat cancer.








can articles like this be re-printed in local newspapers?