Balance is a complex and multi-faceted issue, and disorders can be due to one or more subtle conditions. Testing is vital to achieving accurate diagnosis and treatment: Veterans suffering from dizziness can receive specialized testing to diagnose balance and orientation disorders.
The Center of Balance clinic (COB) at the Northport VAMC is a specialty clinic aimed toward providing a multi-system evaluation of Veterans with complaints of vertigo, dizziness and/or disequilibrium.
Each Veteran undergoes a focused evaluation by an optometrist, audiologist and physical therapist. Our goal is to design, when appropriate, a rehabilitative therapy program to help minimize symptoms and reduce the risk of falls.
Inner ear disorder can cause balance problems
Disorders in the inner ear may contribute to balance problems. Loop-shaped canals in your inner ear contain fluid and fine, hair-like sensors that help you keep your balance.
At the base of the canals are a patch of sensory hair cells. Within these cells are tiny particles that help monitor the position of your head in relation to gravity and linear motion. Examples are going up and down in an elevator or moving forward and backward in a car.
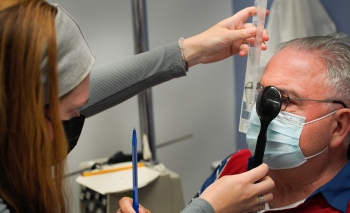
We offer a wide range of highly specialized tests. This is done with goggles fixed firmly over your eyes, tracking and recording your eye movements with camera as you look back and forth between designated points and move your head and body into different positions.
A patient’s eye movements are tracked and monitored via infrared goggles in various conditions. Examples include watching a dot move on a lightbar while lying down and moving into different positions, and while the ear canals are heated and cooled.
The audiologist is looking for any abnormal involuntary eye movements, or what is called nystagmus, to help differentiate between different causes of dizziness.
Computerized test by physical therapists
Physical Therapists utilize a computerized dynamic test in which patients stand on a platform and attempt to maintain balance during brief periods of movement. A safety harness keeps patients from falling.
It is most applicable in situations where balance needs to be followed quantitatively to determine whether a disorder is getting better or worse, or responds to treatment.
These tests are designed to localize and categorize pathological mechanisms of balance disorders.
Balance is complex. The COB clinic doesn’t replace the important medical evaluation that should precede referral to determine other underlying medical causes of vertigo, dizziness and disequilibrium. Still, we are here to help improve our Veterans’ day to day lives as much as possible.
For most of us, vision is a term used to describe how clear things are. In reality, the impact of vision on our lives is much more profound than just the clarity of the images being perceived.
Vision is also connected to our balance system
To maintain balance and navigate space in our physical world, we must organize and integrate information from the visual, proprioceptive and vestibular systems.
A deficiency in any of these three vitals systems can have a dramatic impact on a person’s ability to exist in their world. Visual therapists have many distinct exercises. The skill is knowing when to incorporate the exercises and how to load them.
Because much of the success of the patient lies in developing a better understanding of how to control their visual system, great care must be taken to guide them along the appropriate path so the right neurological patterns are formed.
Key to help for Veterans with balance issues
For Veterans who may be suffering from balance issues, knowing that there is a strong, influential visual component may be the key to getting the help they need.
The COB treatment approach is applicable and offered to all who are suffering from vertigo, dizziness and disequilibrium and have already completed a full medical evaluation.
Some examples of Veterans who may not benefit from the COB are those with a history of Meniere’s disease, microvascular changes/degeneration in white matter, small vessel disease, progressive neurologic diseases (such as Parkinson’s disease) and orthostatic hypotension.
We have had a great deal of success treating Veterans who have suffered a traumatic brain injury, those with benign paroxysmal positional vertigo or neuritis/labyrinthitis, and our aging Veterans to work towards a reduction in falls.
Topics in this story
More Stories
The Veterans self-check assessment takes about 10 minutes to complete and has resources that can help if stress and depression are affecting you.
Nutrition plays an important role in our overall health. Telehealth resources can help you set and achieve your healthy eating goals.
Veterans learn to combine mindfulness with the challenge of climbing.







My daddy had been suffering with this for several years, he’s went every where in the world with no help, most times people just two him go home and fall all you want. Which is so many times a day!! He’s down now than he’s up, and I world live to see him get better
I suffered from vertigo for a long time. A few years ago, I stood up from my chair and the room began to spin. I fell and my head hit the tiles, causing a severe concussion and a mild skull fracture. Even though there was no permanent damage, I knew I might not be so lucky next time. Luckily, I found these powerful vertigo and dizziness exercises and no my vertigo was gone in just days: http://www.healthwise101.com/vertigo-exercises-that-really-work
Been going through this since January, and TIAs. For years.
Does the VA have this Program?
Does the VA have this Program?
How can I get on the waiting list for this program
I had to throw away a pair of Sketchers Memory Foam shoes because the foam was keeping my feet above the floor of the shoe, making me feel like walking on pillows all the time. Got rid if them, balance came right back.