A study by VA’s Million Veteran Program showed that a genetic risk model could accurately predict breast cancer in a large group of women Veterans. The genetic screening tool assesses patients’ DNA for many different genetic variations that, when added together, can elevate a woman’s lifetime risk of breast cancer to 20% or higher, a trigger which usually calls for more actions in current practice.
By scanning a patient’s genome for gene variants using this tool, doctors can create individualized breast cancer screening and risk-reduction plans.
The results appeared in the July 21, 2021, issue of JCO Precision Oncology.
Refining breast cancer screening strategies
Breast cancer is the most common form of cancer for American women. Although mammogram screenings have lowered the number of deaths from breast cancer, better screening methods could help determine risk and help prevent the cancer before it develops, according to the study researchers.
Previous genome-wide association studies – studies that examine the genes of many people for shared traits related to disease risk – have identified multiple gene variations that appear to increase the risk of breast cancer.
While studies have shown that genetic testing for these variations can help predict breast cancer risk, it is less clear whether they would be as accurate for women Veterans. Veterans experience different environmental exposures and psychological stressors than the general population because of their military service, which may affect disease risk.
Developing specific screening plans
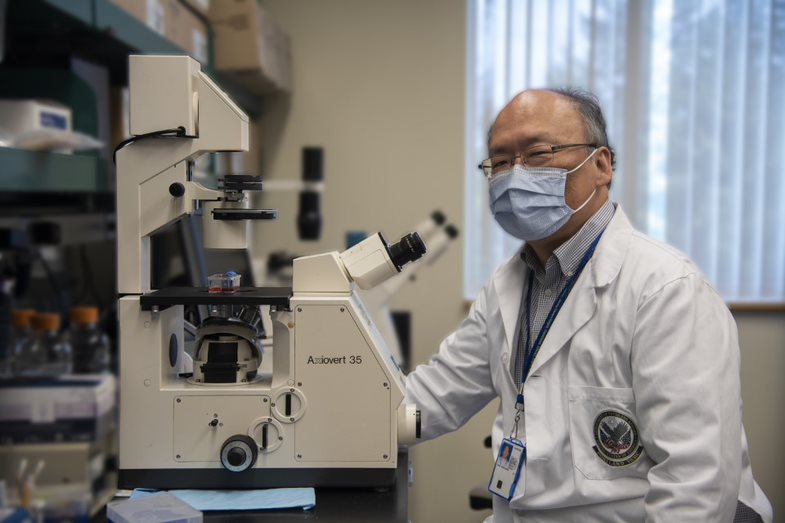
By evaluating women Veterans’ individualized genetic risk for breast cancer, specific screening plans could be developed for each patient, according to Dr. Shiuh-Wen Luoh, who led the MVP study. “The goal is to find the right amount of screening that’s not too expensive and not too emotionally burdensome,” explains Luoh, “but also effective at detecting breast cancer early in woman with that specific risk.”
Luoh is a researcher with the VA Portland Health Care System and the Knight Cancer Institute at the Oregon Health & Science University. Dr. Sally G. Haskell of the VA Women Veterans Health Care program and Dr. Cindy Brandt, both with the VA Connecticut Health Care System and Yale University, co-led the research project.
If genetic testing can help determine a woman’s risk for breast cancer, then prevention and screening measures can be tailored to her needs. “Some women may need a mammogram more frequently than every one to two years,” says Luoh. “For others, in addition to mammogram, they may need abbreviated MRI, a shorter form of the scan that studies have shown could be effective and less expensive than a full MRI. Maybe some women may need less frequent screenings and/or don’t need to begin regular mammogram screening until later if their risk is lower.”
More than 35,000 women Veterans
To better home in on these specific risk factors, Luoh and colleagues turned to a tool called the Individualized Coherent Absolute Risk Estimator (iCARE). iCARE, developed outside VA, is a computer program that allows researchers to build and evaluate models of risk based on multiple data sources. The models can then be used to estimate an individual’s risk of developing a disease.
The researchers used iCARE and incorporated a model of breast cancer genetic risk based on 313 single-nucleotide polymorphisms. A single-nucleotide polymorphism is one genetic variant at a specific location on the DNA molecule. The variants used in the model have previously been shown to modify breast cancer risk.
Luoh’s team applied the prediction model to the genomes of more than 35,000 women Veterans who had volunteered for MVP. Of those, 338 developed breast cancer during an average follow-up of four years. The screening tool proved to be highly accurate at predicting breast cancer risk, especially in women with European ancestry. Because more data is available on this population than for women of African ancestry or other minority groups, the results cannot be generalized to all populations.
Veterans interested in enrolling in MVP can learn more by visiting mvp.va.gov or calling 866-441-6075.
More Information
Click here to read the full story.
Click here to learn more about VA research.
Topics in this story
More Stories
In a new series that highlights advancements in VA health care, VA researchers and clinicians are appearing on a Veteran-themed media platform—Wreaths Across America Radio—to tout their critical work.
Recently published findings from the VA Disrupted Care National Project [...]
Diverse representation of women in health care research allows MVP to make discoveries for women’s health