After being diagnosed with throat cancer at the age of 53, Army Veteran Arthur Daniels needed a total laryngectomy to save his life. The operation would remove his larynx (voice box) and separate his trachea (airway) from the mouth and nose. He would have to breathe through a small hole in his neck known as a tracheal stoma.
Without the ability to close the vocal cords, many patients like Daniels lose the ability to smell and taste, have difficulty lifting objects, and in some cases, have difficulty swallowing food or liquids. But the most difficult part for Daniels was overcoming losing the ability to speak using his vocal cords.
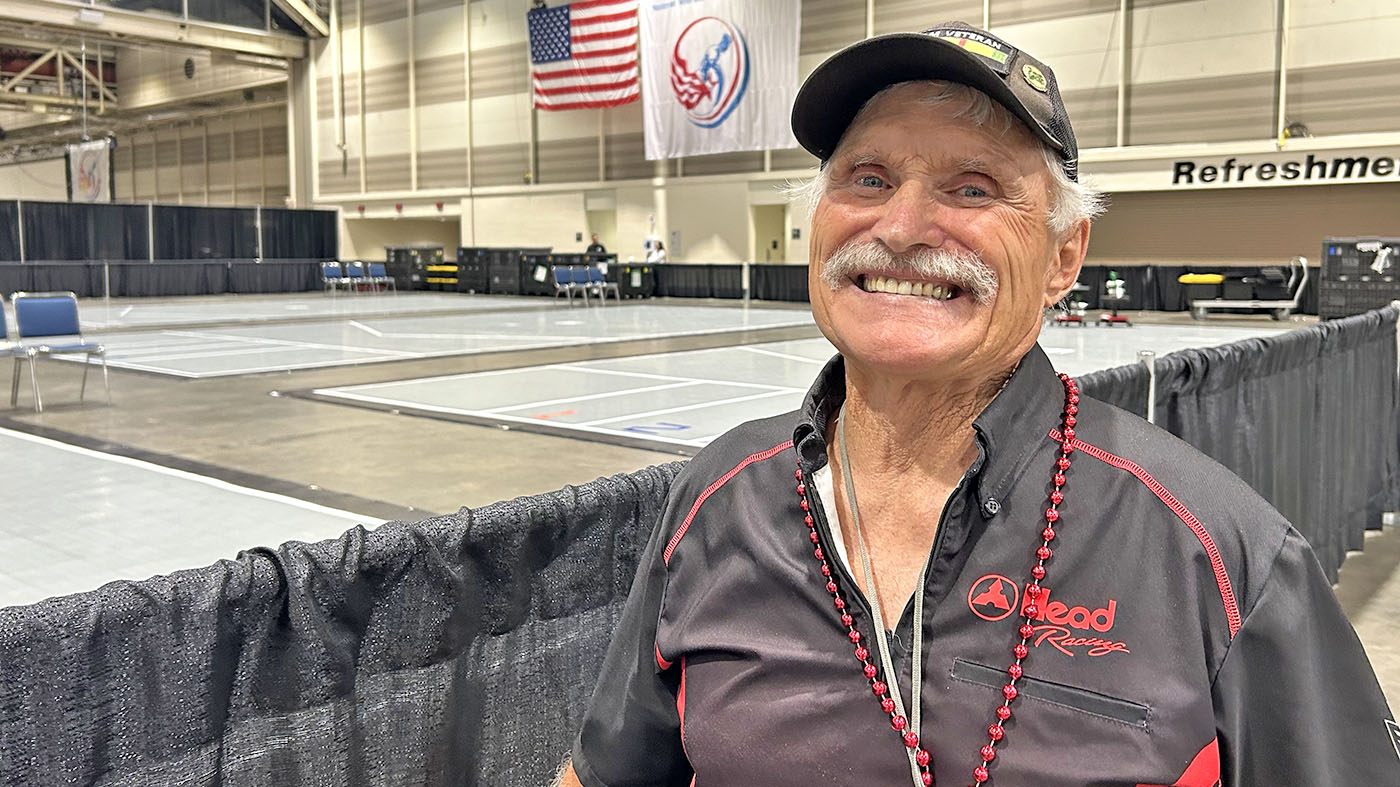
“The first year, I was in a real funk,” he said. “I was vain and the operation changed the way I looked. It was only after I met another cancer survivor who took the time to help me that I felt better. That’s when I stopped feeling sorry for myself.”
The laryngectomy changed more than his looks, though. It also changed his life. “It changes so much,” he said. “The way you speak, smell, swallow. It changed my entire lifestyle.”
Veterans have access to wide range of communication devices
“I used to have a commanding voice,” Daniels said. “I woke and I couldn’t even whisper. The transition was tough, especially because the work I do requires so much communication through talking.”
Veterans who undergo this procedure have several different options to regain their voice. In Daniels’ case, his surgeon placed a small opening between the trachea and the esophagus.
Then, a small, round, plastic tube (an artificial larynx) was inserted to keep the hole open and to allow air to flow into the esophagus. The air then vibrates the top of the esophagus to create a sound for speaking.
After surgery and recovery, Daniels was able to successfully return to work in the engineering service of the Gainesville VA Medical Center.
In addition to the physical demands of being an engineer, Daniels has to very carefully avoid dust and fumes from entering his lungs when working. He protects himself by placing a small filter, known as a heat and moisture exchange, at the stoma, which is designed to replicate the functions of the nose.
“Veterans are very fortunate to have access to a wide range of communication devices and supplies to assist with communication and breathing,” said Paula Sullivan, a speech pathologist and member of the head and neck cancer team at the Gainesville VAMC. “Mr. Daniels has demonstrated the ability to return to an active work and social lifestyle. Arthur is an ideal patient. I love this man. He is doing more than taking care of himself. He is taking care of others.”
“I tell other Veterans it will be fine.”
Following his surgery, Daniels continued to go out of his way to talk with and encourage other Veterans scheduled for a laryngectomy and provides support after surgery.
“I tell them this is not good or bad, it’s just different,” he said. “Sure, some people choose not to understand people like me when we have to use an artificial voice. Or they are not patient as we communicate, but that happens everywhere. We often discount people in life if they don’t talk the way we want, if they use incorrect words or have an accent we don’t like. I tell other Veterans that it will be fine. We just drive on.”
Sullivan is thankful for Daniels’ willingness to volunteer, noting that Veterans always appreciate the opportunity to talk to someone who has experienced the same surgery and the challenges in recovery.
She added that Daniels is available around the clock to meet with a patient or family members and she is eternally grateful for assistance.
Today, Daniels continues to give back to fellow Veterans who are battling throat cancer using his recovery journey to encourage, inspire and uplift patients and their family members.
VA’s speech-language pathology services
VA offers comprehensive speech-language pathology services to Veterans and service members.
Services include early identification or screening, evaluation and treatment for speech, swallowing, language, voice and cognitive-communication disorders.
Topics in this story
More Stories
One strategy credited for the improvement is a focus on building trust and stronger patient-provider relationships.
Army and Marine Corps Veteran started making models after being hospitalized at Connecticut VA.
Veteran Hank Ebert is a bit of a superstar in the National Veterans Wheelchair Games. He has been attending since 1993.