Veteran patient Ralph Kolesar was diagnosed with both obstructive and central sleep apnea in 2014. Since this diagnosis, he has been dependent upon his positive airway pressure (PAP) machine to help him breath better at night.
“Recently, my provider told me about a new procedure VA was doing and determined I would be a good candidate for it,” Kolesar said. “I think that I’m still adjusting to the device, but overall I am getting better quality sleep.”
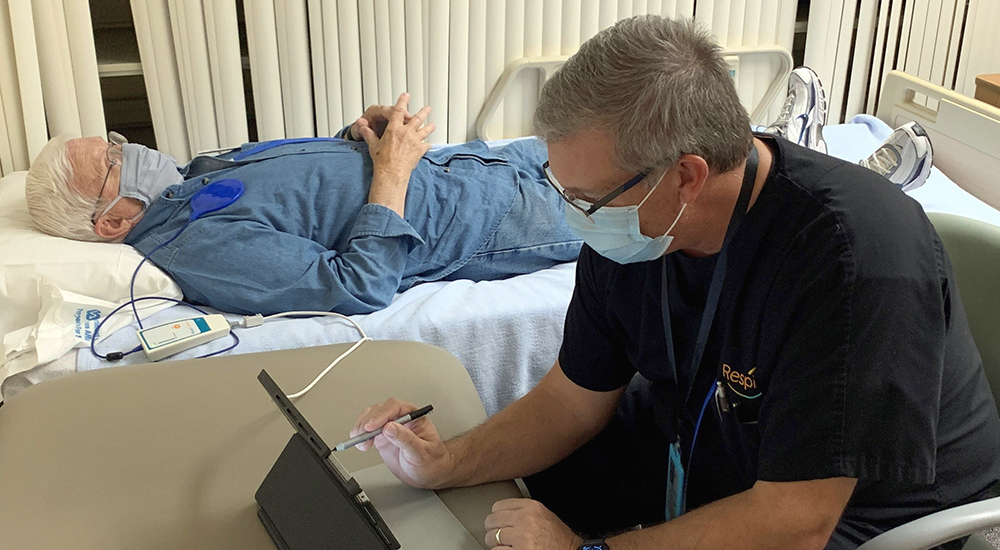
Kolesar had a diaphragm stimulator implanted in September 2021 to help improve his quality of sleep. He has been following up with his providers to ensure that he is healing well and to adjust the amplitude of the device.
“The diaphragm stimulator is a relatively new technology and is available to Veteran patients with moderate to severe central sleep apnea,” said Dr. Susheela Hadigal, pulmonologist. “Once the device is implanted, it takes about six weeks to study the patient’s sleep patterns and to appropriately activate the device.”
According to the CDC, central sleep apnea is a serious breathing disorder that disrupts normal breathing patterns during sleep and has been shown to negatively impact quality of life and heart health.
“I am hopeful that I’ll permanently be off my PAP machine,” Kolesar said. “My CPAP machine has been my life support for so long.”
The diaphragm stimulator is an implantable device that simulates the phrenic nerve (nerve in the chest) to send signals to the diaphragm (the large muscle that controls breathing). The signals stimulate breathing in the same way that the brain stimulates breathing. The device works continuously and automatically monitors and stabilizes breathing patterns, restoring sleep throughout the night.
“Veteran patients who experience difficulty sleeping are referred for a sleep study by their provider and the results of the sleep study help to determine whether a consult with cardiology should be made for the procedure,” Hadigal added.
Sufficient sleep essential for healthy lifestyle
Dr. Hadigal further explains that sufficient sleep is essential in maintaining a healthy lifestyle. Identifying the type of sleep apnea the patient has is also an important step for treatment of the disease.
“There are two kinds of sleep apnea,” Hadigal continued. “Obstructive sleep apnea and central sleep apnea. Obstructive sleep apnea indicates there is an obstruction in the back of the throat or neck. That can be from an anatomical defect or excess fat around the neck. Central sleep apnea occurs when the brain doesn’t send the proper signals to the muscle that controls breathing.”
Cardiologist Dr. Ramil Goel explains that signs of fragmented sleep patterns, not breathing for a few seconds, or if the patient experiences interrupted sleep, may all be symptoms of central sleep apnea.
“The sleep study helps us to confirm the patient’s diagnosis. It also helps determine if a referral to cardiology is warranted,” Goel said. “Screenings include a frailty screening which picks out patients who might not do well during surgery. It determines whether the patient has had prior devices implanted, such as a cardiac pacemaker. We also conduct an in-depth examination of the patient’s previous cardiac surgeries, if any.”
Patients doing well discharged day after surgery
If the patient is a candidate for the procedure, cardiologists will explain the risks and benefits to the Veteran.
“Typically, the procedure is done in the morning and the patient is monitored overnight,” Goel continued. “If they are doing well, they are released the following morning. They’re scheduled for a follow-up appointment a week later to ensure that everything is healing well.”
To date, North Florida/South Georgia VA has experienced tremendous success in helping Veterans overcome health related challenges due to CSA. Interested Veterans should consult their primary care or lung/sleep physician to inquire about the procedure.
Topics in this story
More Stories
Study underscores important role COVID vaccination can have in protecting Veterans from infection and reducing long-term health consequences
Columbia VA’s robotic surgery teams completed their 800th robotic surgery and are on schedule to hit 1,000 by the end of the year.
In a decentralized clinical trial, Veterans can participate from their own homes or local VA instead of having to travel to a research site.






Obstructive Sleep Apnea
How do I get into this study?
Super information, thank you.
I was astounded to read about this new technology. I have been diagnosed twice with sleep apnea, really bad sleep apnea. I have tried every mask that is made for a CPAP machine and I can’t stand any of them. I get to sleep with one of the masks but about 2 hours later I am awake and ripping it off. I would be a candidate for this new technology. But if you think that’s astounding, read this. I have myasthenia gravis, a rare neuromuscular autoimmune disease. It’s doing its best to kill me and has almost succeeded 6 times. It shuts down the operation of the diaphragm which shuts down the lungs. What if you had a stimulater that could stimulate the diaphragm when it shuts down. I would no longer have to worry about this disease killing me!!! Look into it!!!!!!!
When will this procedure be done all across the system? Approximately 5 years ago I was issued a conventional CPAP unit I tried to assimilate the use of it. Due to the sound and situation with either fitting and or getting tangled in the perifera, hoses and what not. I was subjected to 2 different sinus and rynoplasty procedures any results were negligible.
I’d be uncomfortable having surgery at the VA. Even for SC things I’ve had them done by outside providers.
When can we expect this procedure to be available to veterans in the San Antonio Texas area?
I was diagnosed with severe sleep apnea and use my PAP machine every night. I am a patient at the Seattle VA. Who do I contact to see when or if they will use it here.
If you don’t need the CPAP machine anymore, do you lose the 50% disability for OSA?
Following
Hello Dave, I noted your comment asking if you don’t need the CPAP machine do you lose the 50% disability for OSA. My question if you don’t mind answering it. What is OSA.
Obstructive Sleep Apnea