Drug overdose is a public health crisis that claims more than 96,000 lives every year in America. Opioid overdose account for 67.8% of those deaths.
An overdose occurs when your body is exposed to one or more drugs, in a dosage or combination that it cannot handle. Overdose can lead to permanent damage or death if not treated quickly. The signs and symptoms of a drug overdose depend on several factors like what kind of drugs were consumed, the body’s level of tolerance and if other medications or alcohol were involved.
Drug overdose: The most common things to watch for:
- Loss of consciousness
- Loss of balance
- Slowness of breath or lack of breathing altogether
- Tiny, pinpoint-like pupils
- Pale, blue or cold skin
- Seizure
- Headache
- Chest pain
- Confusion or paranoia
- Snoring or gurgling (snoring can mean that the person is struggling to breathe)
Responding to a drug overdose
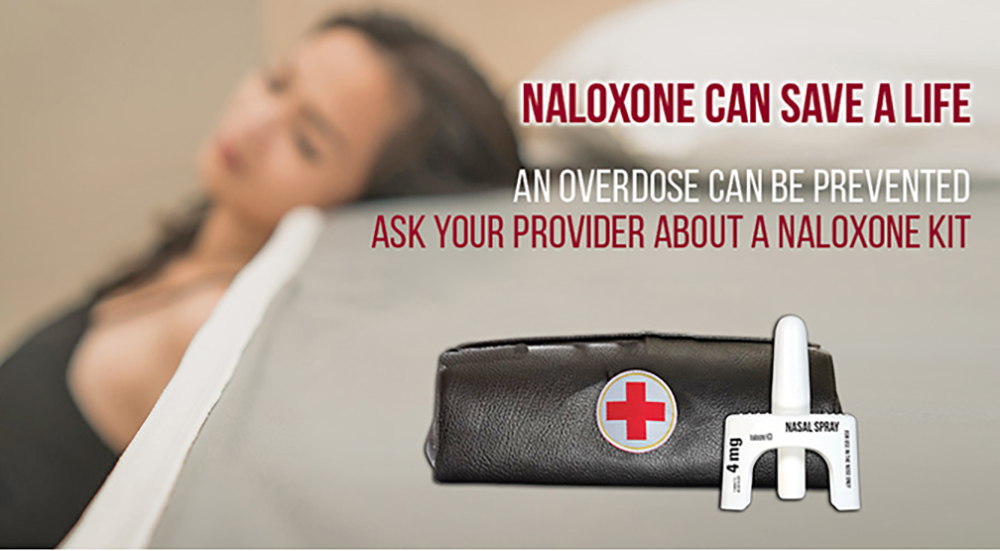
If you or someone around you displays signs of an overdose, call 9-1-1 immediately. The next step is to administer the life-saving drug Naloxone.
“Naloxone rapidly reverses the overdose by blocking the effects of opioids,” said Dr. Edward Radden III, medical director of the Substance Abuse Prevention Program at the Washington DC VA. “Everyone should have one of these on hand if you or someone you know use opioids.”
Naloxone comes in an easy-to-use nasal spray and can be picked up for free at any VA pharmacy by eligible Veterans. It is also free to the public at any DC pharmacy. No prescription or ID is needed. Learn more about Naloxone here.
Along with Naloxone, VA provides Veterans struggling with addiction multiple recovery programs that include:
- Cognitive Behavioral Therapy
- Motivational interviewing
- Motivational enhancement therapy
- Medications
- Support groups
Intensive program
Radden’s team of health care professionals lead a 10-week intensive outpatient program. At any given time, he said they are helping a couple hundred Veterans in DC, Virginia and Maryland break their addictions.
“Our intensive outpatient program, which would cost hundreds of dollars a week outside of VA, is free for eligible Veterans,” said Radden. “When paired with our opiate treatment program, we can really help you overcome your addiction.”
The opiate treatment program provides daily doses of methadone to help curb cravings and get Veterans through withdrawals from drugs like fentanyl, heroine or oxycodone. Currently, there are about 140 Veterans in Washington DC VA Medical Center’s methadone clinic, making it the third largest in the VA’s system.
Despite the numbers, Radden said they don’t put Veterans on a waiting list for access to care.
“About 25% of our program participants are here for opioid use disorders, which carry with it a high-risk of overdose. We want to get them immediate treatment. If you need assistance, just show up. We will help you. There’s no reason not to get treatment today.”
Learn more about VA’s Substance Abuse Prevention Program.
Topics in this story
More Stories
The Medical Foster Home program offers Veterans an alternative to nursing homes.
Watch the Under Secretary for Health and a panel of experts discuss VA Health Connect tele-emergency care.
The 2024 National Veteran Suicide Prevention Annual Report provides the foundation for VA’s suicide prevention programs and initiatives.






YOU NEED TO GIVE DETAILED INFORMATION ON HOW A SERVICE CONNECTED VETERAN CAN GET THIS PRODUCT AT A VA PHARMACY.