Simulation learning brings a unique hands-on experiential component to health professions trainees (HPTs) long before they touch a patient. Skills that were once only practiced on real patients at the bedside—such as performing complex medical procedures like intubation or surgery—are now trained in high-tech simulation centers at VA facilities across the country.
Simulation creates a learning environment where mistakes are embraced and even encouraged. In this safe learning environment, HPTs practice skills repeatedly, learning from their mistakes and correcting them before they perform the procedure on a patient, thus enhancing patient safety.
This freedom to and encouragement of making mistakes through simulation training is beneficial in surgical settings, particularly robotic surgery, where the stakes are high and mistakes could be costly.
“A lot has changed in understanding the way that simulation can actually help protect patients,” said Dr. Angela Guzzetta, chief of Bariatric Surgery, North Texas VA and director of Simulation for General Surgery at the University of Texas Southwestern. “The best thing about doing practice in a simulation is that it’s low stakes and mistakes don’t have the same consequences. We want residents to make those mistakes in simulation so they learn and correct and then do better.”
Simulation has become standard part of surgical training

Simulation learning provides a safe place to practice and master skills that previously could only be practiced bedside.
For surgical residents specializing in robotic-assisted surgery, simulation has become a standard part of their surgical training. They spend hours practicing on the simulation robot to build their surgical skills. Residents practice in the simulation lab at UT Southwestern and on the simulation console at Dallas VA.
“The robot is totally different than anything else the residents use in training. It does have nuances on how to use it,” said Guzzetta. She explained the muscle memory residents must develop in using the robot is like learning how to operate a car. When driving, the driver should not be thinking about where the turn signal is or how to turn the wheel but should be focused instead on where they are driving.
“What we’ve done is just take driver’s ed and put it right into the resident lounge so they can practice and get those deliberate repetitions that make surgery safer for patients,” she continued.
Attending surgeon can instantly take control of robot
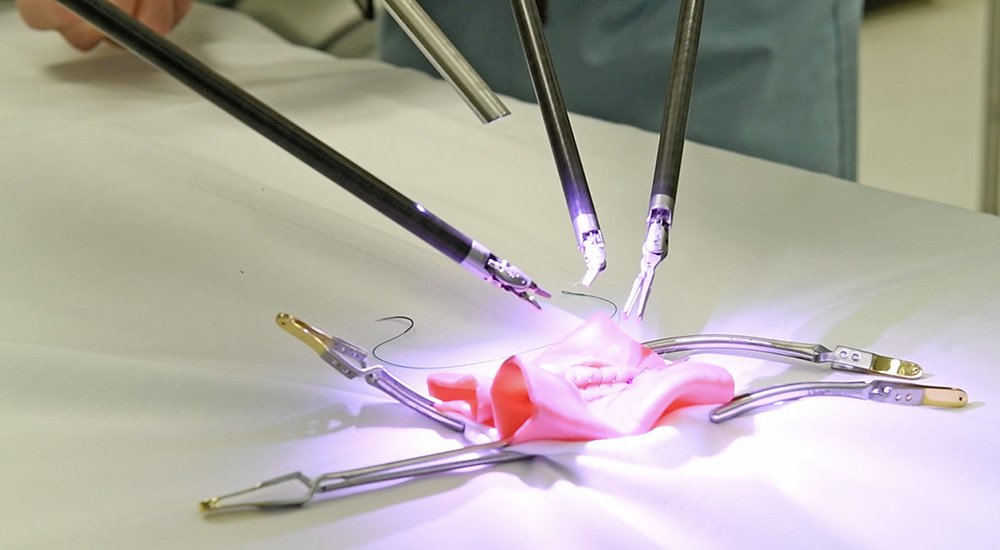
Surgical residents who have advanced in their training will then perform surgeries under the supervision of an attending surgeon using one of Dallas VA’s three da Vinci dual console robotic systems. These systems have 3D vision of the operating area and audio allowing the surgeon to communicate with assistants in the operating room.
Through the console, the surgeon controls articulated robotic arms to perform the surgery, which provide for increased range of motion and tactile response.
With the dual console system, the surgical resident sits at one console performing the surgery while their attending surgeon sits at the second console overseeing the resident’s movements. If the resident needs help during the procedure, the attending surgeon can instantly take control of the robot with the push of a button to perform part of the surgery while also teaching the resident.
The seamless transfer of control during surgery enhances patient safety in the OR while allowing residents to have a deeper level of involvement in surgical procedures.
Learn without a break in the surgery
“It makes a big difference being able to push a button and trade back and forth during the surgery compared to laparoscopic surgery where it is a big process to switch for the surgeon to show the resident what they want and then switch back,” said Dr. Cortland Polley, surgical resident at Dallas VA. “It is good for us trainees to be able to both learn and see what the attending wants us to do without a break in the surgery.”
During VA Health Professions Education Week, March 13 – 17, VA recognizes the more than 118,000 HPTs who train each year in VA and the more than 1,400 educational institutions that partner with VA to train future health professionals.
These academic affiliations, some of which began more than 75 years ago, are coordinated by VA’s Office of Academic Affiliations (OAA). Find out more about VA’s academic mission by watching this video and visiting the Office of Academic Affiliations website.
Topics in this story
Link Disclaimer
This page includes links to other websites outside our control and jurisdiction. VA is not responsible for the privacy practices or the content of non-VA Web sites. We encourage you to review the privacy policy or terms and conditions of those sites to fully understand what information is collected and how it is used.
More Stories
Special event provided essential baby items and resources for expecting women Veterans in Texas.
As of July 2024, VA has approved more than 1.1 million claims made through the PACT Act. VA leads the way in exposure-informed care.
A story of family, legacy and the enduring bond between a father and son at the Golden Age Games.






The VA should provide free BLS / ACLS / PALS / ATLS training and Certifications to its Veteran physicians through TMS.