Uterine cancer, also called endometrial cancer, is the most common gynecological cancer, and it affects more than 800,000 people in the United States.
There are no screening tests for uterine cancer in those who do not show symptoms. And it’s not tested for during routine exams with your doctor. Even a Pap smear test does not screen for this type of cancer, which is why it’s important to know your body, know the risks and know the warning signs to catch it early.
Am I at risk?
It is not possible to completely prevent uterine cancer. However, being aware of the risks can help you take control of your health and decrease your chances of developing it. The risk of uterine cancer also increases with age—but it doesn’t only occur in people over 50.
Risks may include:
- Age. Uterine cancer primarily affects women who have reached menopause or are in their postmenopausal years. But this is not always the case. Women can develop it at any age.
- Obesity. Being overweight or obese is associated with a higher risk, because fatty tissue in people who are overweight produces additional estrogen, which increases your risk.
- Diabetes. Elevated insulin levels and insulin resistance, common in diabetes, can lead to an imbalance in other hormones. This can promote the growth of uterine cells potentially leading to the development of cancer.
- High blood pressure. Studies have suggested that women with chronic hypertension may be at higher risk.
- Polycystic ovary syndrome (PCOS). PCOS can elevate your risk, as it’s often associated with hormonal imbalances and irregular menstrual cycles.
- Family history of cancer. Having a close relative such as a mother or sister who has had uterine cancer increases your likelihood of developing the disease. Genetic factors can play a role.
- Hormone therapy, such as tamoxifen. Hormonal imbalances can disrupt the normal growth and shedding of the uterine lining.
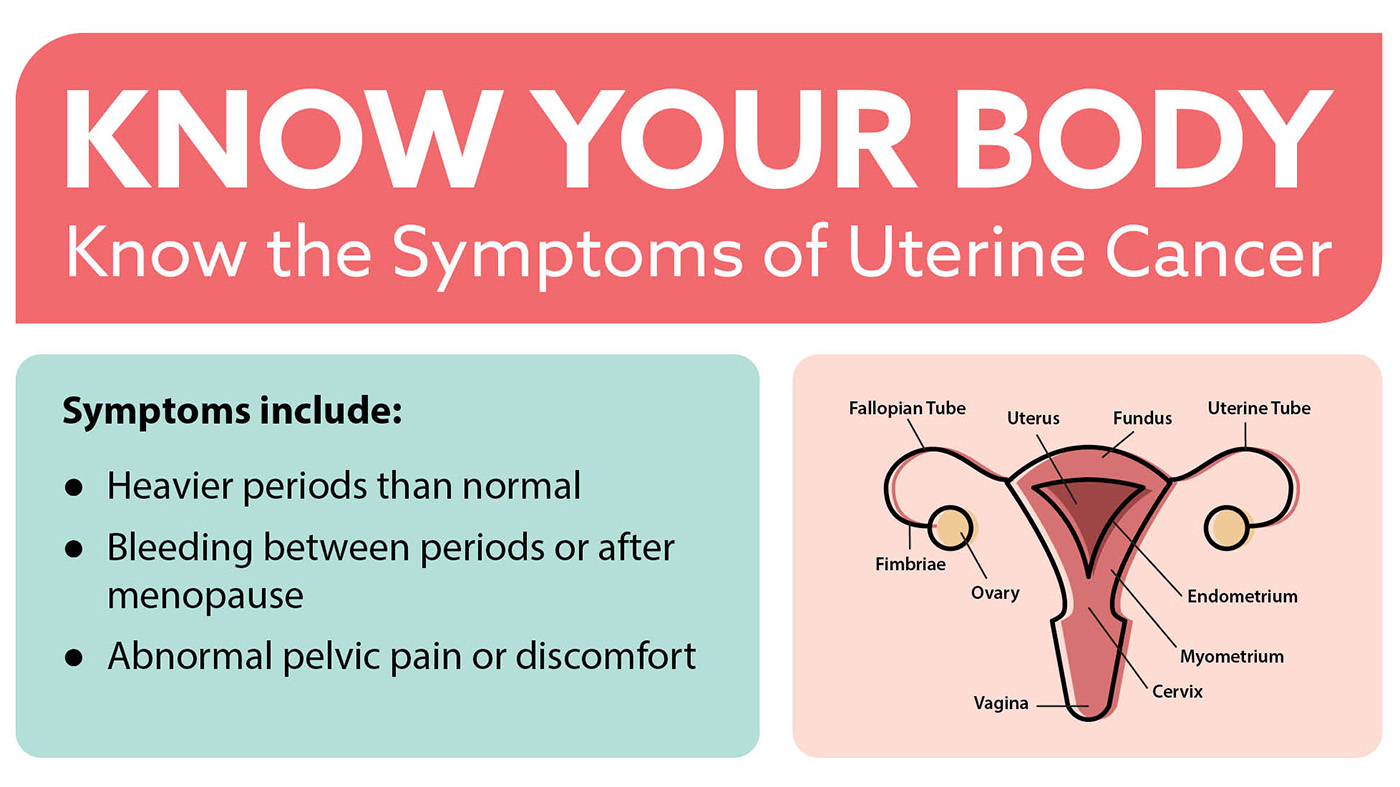
What symptoms should I look out for?
If you notice unusual vaginal discharge or abnormal bleeding, it could be a warning sign of uterine cancer. It is not normal to have heavy bleeding, bleeding between periods or any bleeding after menopause. Even just one dab of blood after menopause is enough to raise concerns with your doctor. Uterine cancer may also cause symptoms such as abnormal pain, pressure or discomfort in your pelvis. If you’re experiencing any of these symptoms, reach out to your VA health care team right away.
What else should I know?
There is a significant racial disparity in survival rates of those with endometrial cancer. Black people are twice as likely to die from uterine cancer than people of other races, no matter what stage or subtype of uterine cancer they may have. Black people are also more likely to have uterine fibroids. Ultrasounds are not always helpful, so you should talk to your doctor about endometrial sampling if you’re concerned.
How do I test?
Talking about these types of concerns is never easy, but know that VA is here to answer all your questions and help you address any worries you may have. You have access to primary and gynecological care at VA (including Pap tests and HPV vaccines). If something does not feel right, don’t hesitate: contact your VA health care team right away. If you have symptoms, VA can provide tests, such as an ultrasound or biopsy to detect or rule out cancer.
Remember early detection matters and uterine cancer is usually treatable if detected early.
Read here for more information and here to learn more about uterine cancer.
To read more stories on VA’s cancer research and treatment, visit VA News and Information.
Topics in this story
Link Disclaimer
This page includes links to other websites outside our control and jurisdiction. VA is not responsible for the privacy practices or the content of non-VA Web sites. We encourage you to review the privacy policy or terms and conditions of those sites to fully understand what information is collected and how it is used.
More Stories
The Medical Foster Home program offers Veterans an alternative to nursing homes.
Watch the Under Secretary for Health and a panel of experts discuss VA Health Connect tele-emergency care.
The 2024 National Veteran Suicide Prevention Annual Report provides the foundation for VA’s suicide prevention programs and initiatives.