VA experts in artificial intelligence are teaching computers to think like “perfusionists” – operating room staff who work heart-lung machines during surgery.
Doctors often stop a patient’s heart during a major cardiac surgery. In this situation, a perfusionist operates a heart-lung bypass machine. The machine supplies needed blood and oxygen to the patient whose heart is on hiatus.
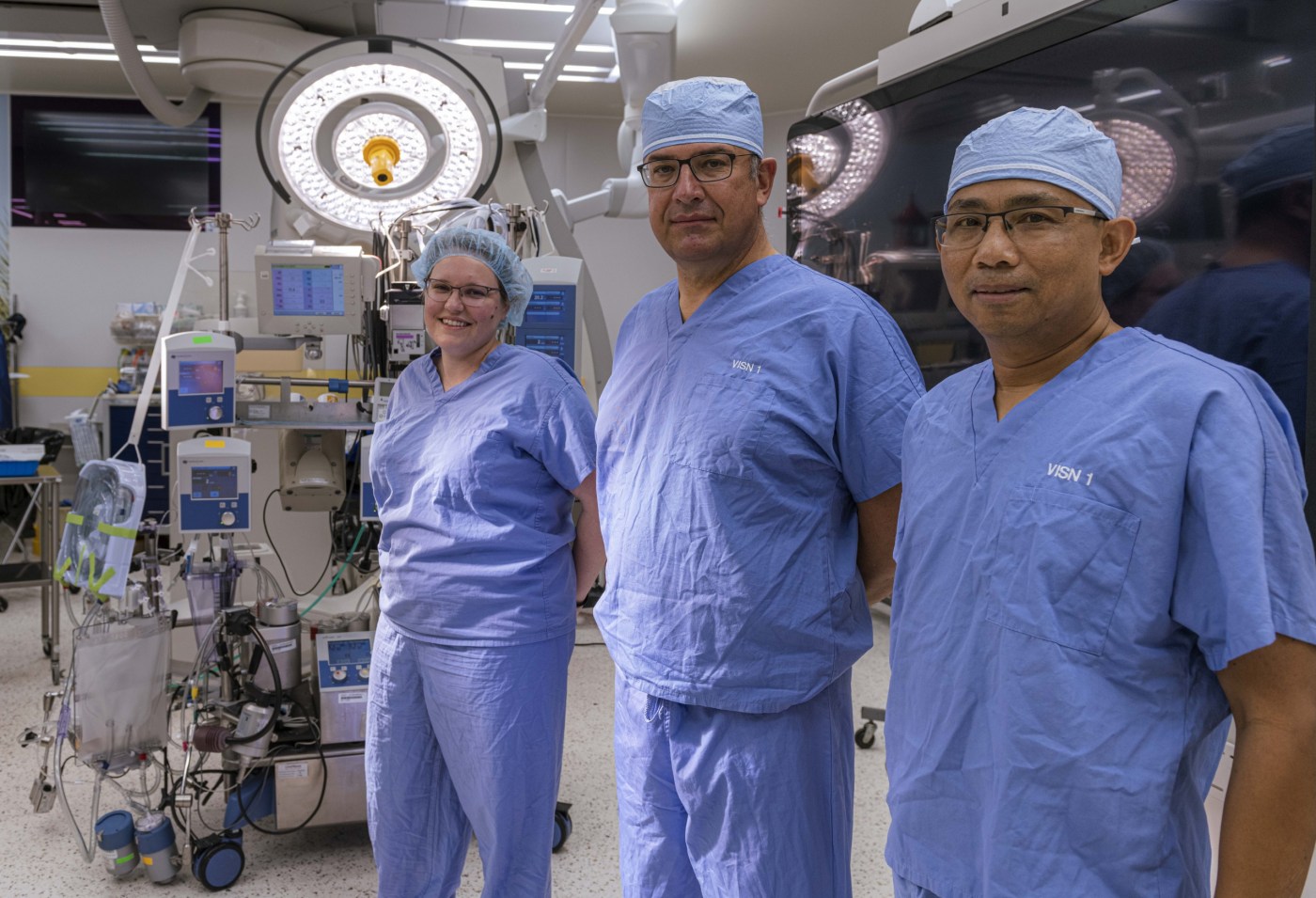
In a paper titled, “Using Machine Learning to Predict Perfusionists’ Critical Decision-Making During Cardiac Surgery,” researchers from the VA Boston Healthcare System, Harvard Medical School, Brigham and Women’s Hospital and Georgia Tech University detail their progress toward a computer-based system to help perfusionists in the OR make critical decisions as they operate the bypass machine.
They presented the paper in September 2021 at a meeting of the Medical Imaging Computing and Computer Assisted Intervention Society.
Supporting perfusionists when the pressure’s on
Within VA and at other health facilities across the country, recent decades have seen sophisticated technologies enter the operating room. And growing numbers of medical specialists harmonize their roles in caring for patients. While these systems have improved patient health, they can also add to the pressure on OR staff.
In this pressure-cooker environment, the perfusionist must make quick and accurate decisions in managing the heart-lung (cardiopulmonary) bypass machine, says Dr. Marco A. Zenati, the study’s lead investigator. Zenati is chief of the Division of Cardiac Surgery at the VA Boston Healthcare System and a Harvard Medical School professor of surgery.
Even expert perfusionists can become overwhelmed, given the demands on them, says the physician-researcher, who leads the Medical Robotics and Computer-Assisted Surgery Lab at the Boston VA and Harvard. A computerized system to partner with perfusionists can improve patient safety, he says. This can potentially avoid adverse events such as kidney damage or a blood clot from heart-lung bypass.
Preparing computers to pick up patterns
Dr. Lauren R. Kennedy-Metz, a paper author and Harvard Medical School surgery instructor, likewise emphasizes the project’s importance. “The patient is at the mercy of the cardiopulmonary bypass machine during heart surgery, and a lot of pressure is on the perfusionist to make decisions in operating this really complex machine,” says Kennedy-Metz, a member of Zenati’s VA-Harvard lab. “The goal of this project is to apply a form of artificial intelligence called machine learning to make recommendations that perfusionists can rely on along with their own expertise.”
Veterans are among those who stand to benefit most. They may be especially susceptible, explains Kennedy-Metz, to adverse events during cardiac surgery, as they are often older and have conditions such as diabetes. Kennedy-Metz says she is proud of VA’s contribution to this study, including its role as the site for all data collection. She points to her VA site in Boston, where the study was based, as a prime example of leadership not only in this study, but in “a steady stream of highly impactful research.”
For perfusionists, one responsibility among many is to monitor the delivery of oxygen (DO2) while the patient is connected to the bypass machine. When DO2 falls below the threshold of 280 ml/min/m2, the patient is at risk for complications. The study focused on perfusionists’ responses to these dangerous dips in DO2. The goal is to enable computers to make decisions like master perfusionists – but without the strain that can undermine human judgment.
More Information
Click here to read the full story.
Click here to learn more about VA research.
Topics in this story
More Stories
In a new series that highlights advancements in VA health care, VA researchers and clinicians are appearing on a Veteran-themed media platform—Wreaths Across America Radio—to tout their critical work.
Recently published findings from the VA Disrupted Care National Project [...]
Diverse representation of women in health care research allows MVP to make discoveries for women’s health






IT’S A REALLY GOOD, AND SAFE IDEA.
I recently had open heart surgery at the TAVR Clinic of Sutter Hospital in Sacramento, CA. I found this article extremely interesting since I was on the heart – lung machine for a total of 3 hours.
PRE-PROCEDURE DIAGNOSIS: Rheumatic mitral valve disease, unspecified. Atherosclerotic heart disease of native coronary artery without angina pectoris. Unspecified atrial fibrillation.
PROCEDURE(S) PERFORMED:
MULTIPLE CORONARY ARTERY BYPASS X3, WITHLAFT IMA AND RIGHT GREATER SAPHENOUS VEIN GRAFT, ENDOSCOPIC VEIN HARVESTING, MITRAL VALVE REPLACEMENT WITH 33MM ST JUDE EPIC VALVE, LEFT ATRIAL APPENDAGE EXCLUSION WITH 50MM CLIP, BILATERAL PULMONARY VEIN ISOLATION TRANSESOPHAGEAL ECHOCARDIOGRAPHY.
My surgery was very successful and I am well on my way to full recovery.