VA has adopted several initiatives through its Whole Health wellness program using a variety of Complementary and Integrative Health (CIH) practices designed to keep people well, in addition to supporting recuperation and healing.
In some cases, it can result in a reduction in medications. For many Veterans, it’s changing their lives.
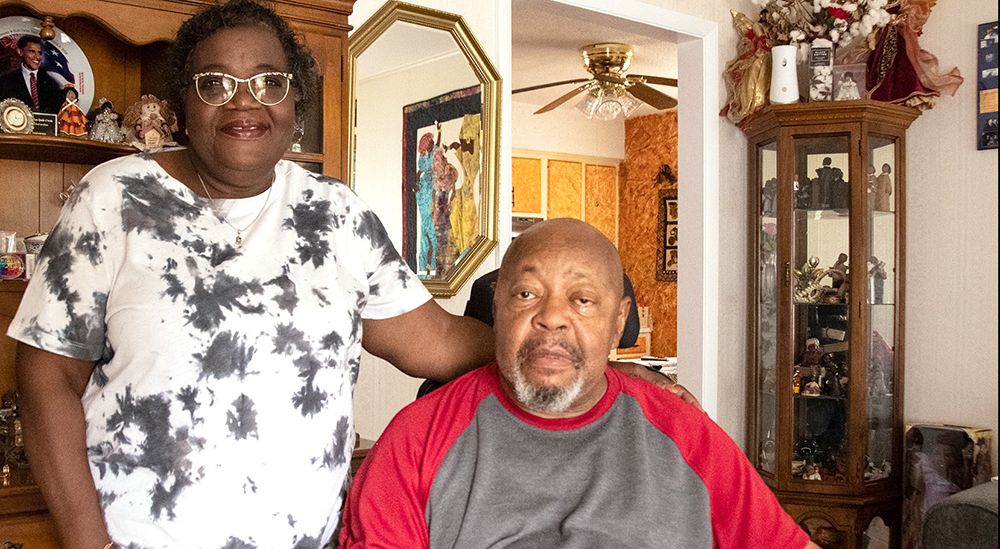
Veterans are aware of the need for good health. Some are making changes subtly over time and others are making daily changes. For Wavey Alston, a Vietnam-era Air Force Veteran, change began in June 2017.
“I just couldn’t live with the back pain much longer,” said Wavey. “I was taking Morphine tablets, and they helped, but I only felt better until the effect wore off and the pain came back.”
VA replaced morphine with acupuncture
Wavey’s back pain began in the Air Force. While stationed in Thailand during the Vietnam War, he worked as an aircraft mechanic, which required much physical labor.
“I had fun,” said Wavey, “But I did a lot heavy lifting. Of course, I was young and it didn’t seem to be a problem then.”
Wavey returned home to Durham, N.C., and found work at a printing company. The years of heavy lifting began to emerge in the form of back pain.
“My back just got worse,” said Wavey. “Then our insurance costs went up. I never considered going to VA until then but it was the best decision we ever made.”
Wavey became a patient at the Physical Medicine and Rehabilitation Clinic at the Durham VA. He acknowledged his dependency on opioids to control pain. To him, the morphine tablets were necessary but self-defeating. The staff at the clinic suggested a possible alternative: acupuncture.
“Needle thing put me off but glad I stuck with it”
Acupuncture is a CIH practice involving the insertion of needles at strategic points on the body. It is traditionally and frequently used to treat pain. Studies show that acupuncture is an effective treatment for various conditions, especially chronic back pain. Despite the uneasiness some Veterans initially feel about the use of needles, acupuncture is a relatively painless alternative treatment option that promotes wellness.
“The whole needle thing put me off at first,” said Wavey. “But the doctors explained the benefits to me and I decided that it wouldn’t hurt to try it.” It took a few visits but the treatments began to work. “It was a strange feel at first.” He was seeing an acupuncturist twice a week. “It took a while to start feeling the benefits,” said Wavey. “I’m glad I stuck with it.”
Wavey has engaged in acupuncture for his chronic back pain for the past four years. While his pain is not gone entirely, it is not the hurdle that it once was.
“Before I started all this, I could barely move without the morphine,” he said. “It was that bad. Now, I can move around and do more of things that I couldn’t do before. Can’t say I’m a new man, but I really feel like it.”
Topics in this story
More Stories
Bob Jesse Award celebrates the achievements of a VA employee and a team or department that exemplifies innovative practices within VA.
The Medical Foster Home program offers Veterans an alternative to nursing homes.
Watch the Under Secretary for Health and a panel of experts discuss VA Health Connect tele-emergency care.







I didn’t know that acupuncture was offered by the VA, I’ve been using opioids for over 25 years. I’m taking something else now that is akin to methadone but still contains some opioids. Who would I check with to see if my VA in Fresno offers acupuncture? I would like to get off of what I’m taking now, still have pain, maybe this would help me.
I can attest to the success of acupuncture treatments. As a wounded/disabled Vietnam Vet my wife and I while we were living and working abroad in the 80’s entered a certification program in Singapore. Our goal at the time was just for her to expand her med skills.
We had no idea if acupuncture would help me or at least reduce my need for opiates. If it was on the VA radar I never heard about it before now. Big believer for the last 30 years.
Glad to see VA on board.
Nothing in the article suggests the presence of opioid addiction, or even habituation prior to the use of acupuncture. The “dependence” described appears to refer to the effectiveness of morphine in relieving pain, consistent with its expected duration of action. The use of acupuncture in this patient appears to be effective and should be continued in lieu of opioids. Hopefully the acupuncture will be effective over the long term. However, should the pain fail to respond to acupuncture and possibly other non-opioid interventions in the future, the reintroduction of an opioid should again be considered; it may end up being the intervention of choice.