Experiencing the concluding chapter of life can be difficult for patients and those who care for them. But, Dr. Pamela Steadman-Wood, a clinical Geropsychologist at Providence VA, believes that there is a special kind of beauty and a significant amount of bravery involved in facing end of life decisions and engaging in open discussions with loved ones and providers.
“Veterans are very familiar with acts of bravery. And being able to open themselves up to talking about death and dying is one of the bravest acts of all time,” she said.
Suicidality vs desire for hastened death
As Veterans approach the end of life, experiencing thoughts about death and dying is normal. For some, thoughts about suicide or a desire for hastened death are prominent. Providers are tasked with making this distinction to best inform interventions.
A Veteran with a desire for hastened death seeks control over the dying process and wishes to accelerate their own death. This often occurs in response to suffering with a life-threatening condition. Veterans who experience thoughts of suicide have thoughts of engaging in suicide-related behavior and may have the intent to die by suicide.
For providers, recognizing risk factors for either suicide or a desire for hastened death is critical. Early detection facilitates appropriate interventions to help save Veteran lives.
“Some of the biggest predictors we see for suicide and a desire for hastened death include depression, poor social supports and the experience of hopelessness,” said Dr. Kristen Dillon, a clinical geropsychologist in Hospice & Palliative Care at Bedford VA. Pain and sleep issues can also be contributors to a desire for hastened death and/or an elevated risk for suicide.
Provider support is available
The Suicide Risk Management Consultation Program (SRM) is a free resource to support providers as they treat Veterans at risk for suicide at the end of life.
SRM is a tool for providers to discuss risk assessment and other best practices. “Risk assessment inherently is a stressful experience. And then you add the complexities of end of life, and you try to tease apart desire for hastened death versus suicidality. The consultation program can be an incredible asset as we providers navigate those nuances and support a Veteran through their final chapter,” Dillon said.
This June, Steadman-Wood and Dillon will discuss suicide prevention and end of life as part of the monthly SRM lecture series. The lecture series occurs on the 2nd Wednesday of every month from 2-3 p.m. ET. Interested VA and community providers can register here to learn more.
Easing the transition
VA and community partners offer an array of resources to help guide and support Veterans as they enter the last chapter of their lives. Some sites to visit for more information and assistance include:
- We Honor Veterans: https://www.wehonorveterans.org/.
- VA Palliative Care: https://www.va.gov/GERIATRICS/pages/Palliative_Care.asp.
- VA Hospice Care: https://www.va.gov/geriatrics/pages/Hospice_Care.asp.
Help is always available. If you are a Veteran in crisis or are concerned about one, call the Veterans Crisis Line at 800-273-8255 and press “1” or text 838255.
The appearance of external hyperlinks does not constitute endorsement by the Department of Veterans Affairs of the linked web sites, or the information, products or services contained therein.
Topics in this story
More Stories
Forget 'No Pain, No Gain'—try 'No Pain, More Gain' with Tai Chi! Calm the mind and gift yourself well-being in this week's #LiveWholeHealth practice.
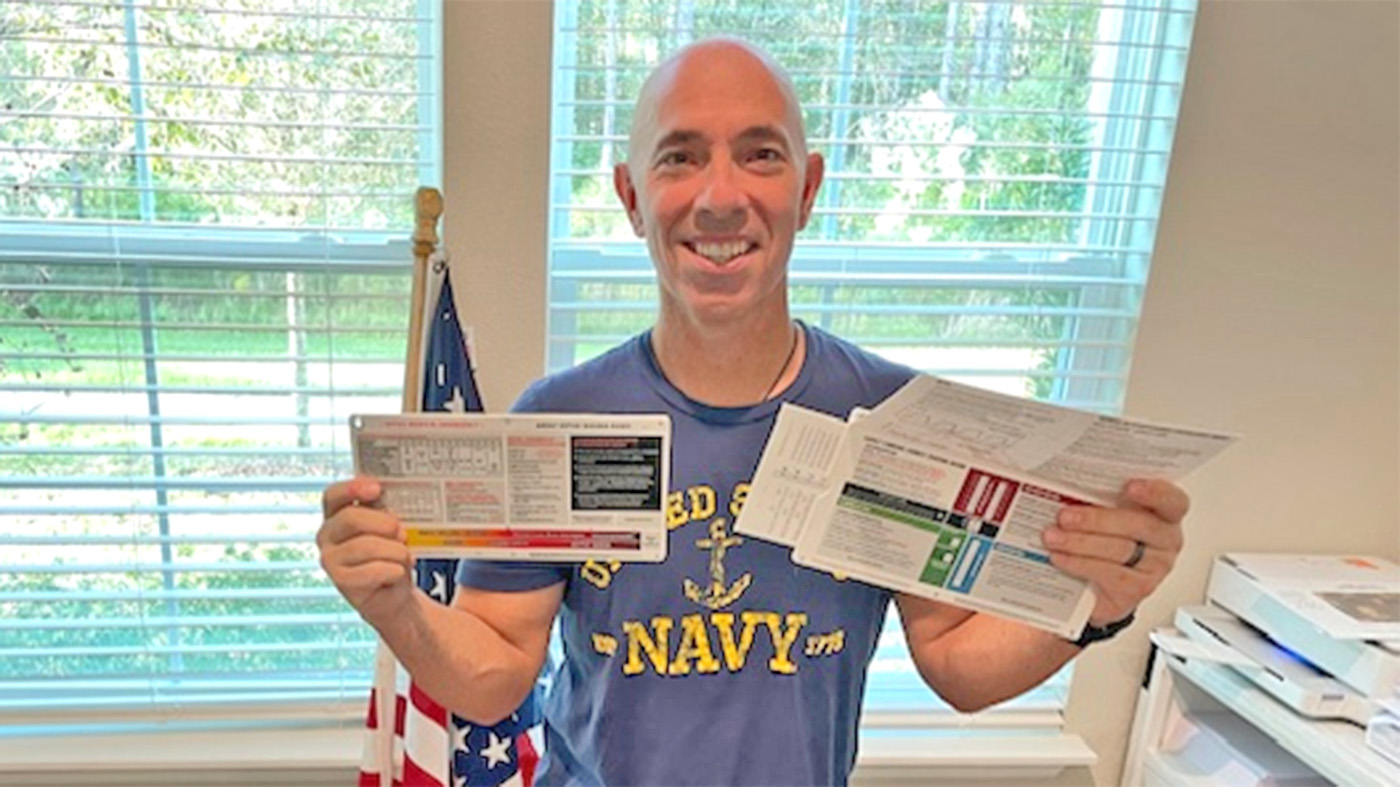
Critical care dosing guides are critical in emergency care where a clinical team’s skill and focus matter most.
Combat Veteran faces the traumatic events of her PTSD during prolonged exposure therapy and looks forward to the days to come.