Alzheimer’s. Dementia. These diagnoses rip the chord of safety and certainty in patients, families and caregivers at an estimated rate of 6.5 million Americans age 65 and older in 2022 and an estimated 168,600 VA patients in 2021. It’s a diagnosis projected to increase to 12.7 million Americans by 2050 and 217,400 VA patients in the next decade alone.
While a diagnosis is frightening enough, so too are distress behaviors that may be associated with the disease, like verbal outbursts, inappropriate behaviors, even physical aggression. These often interfere with medical treatment and caregiving that may harm the patient, the caregiver or the treatment team.
As a young psychologist working at Central Iowa VA’s Community Living Center, Dr. Kathleen Matthews saw these distress behaviors first-hand and realized these Veterans could be better cared for through non-pharmacologic behavior plans rather than the traditional method of psychotropic medications.
Working with team members, she created the Behavioral Recovery Outreach (BRO) team to meet this extremely vulnerable patient population’s unmet needs.
“BRO helps build a sense of connection and shared purpose for meeting these Veterans’ needs,” Matthews said. “By reducing distress behaviors, especially given that BRO Veterans tend to have very severe behaviors, there is a sense of hope that these Veterans can get better to the point where they are able to be discharged from the inpatient setting even if initially it feels hopeless.”
Commitment of BRO teams make care model work
The basic premise is learning about the Veteran as a person and utilizing interventions such as redirecting or offering alternatives to mitigate potential distress reactions. Sometimes it may be as simple as offering a different toothpaste to the Veteran who refuses to brush his teeth, or it may be as complex as convincing the Veteran she has already finished her work for the day if she is fixating on her former career.
While the highly individualized Veteran-centered holistic approach is central to addressing behavior care needs and developing effective behavior plans, it is the commitment of the interprofessional BRO teams that exist at approximately 15 VA facilities—including Minneapolis VA, the second VA site to establish a BRO team—that make this care model work.
Behavioral Neurologist Dr. Jamie Starks is the medical director for the Minneapolis VA BRO team. Her goal is to have all medical personnel at her VA, including the medical residents and students she works with, build empathy for what these Veterans are experiencing and provide a framework of why behaviors occur.
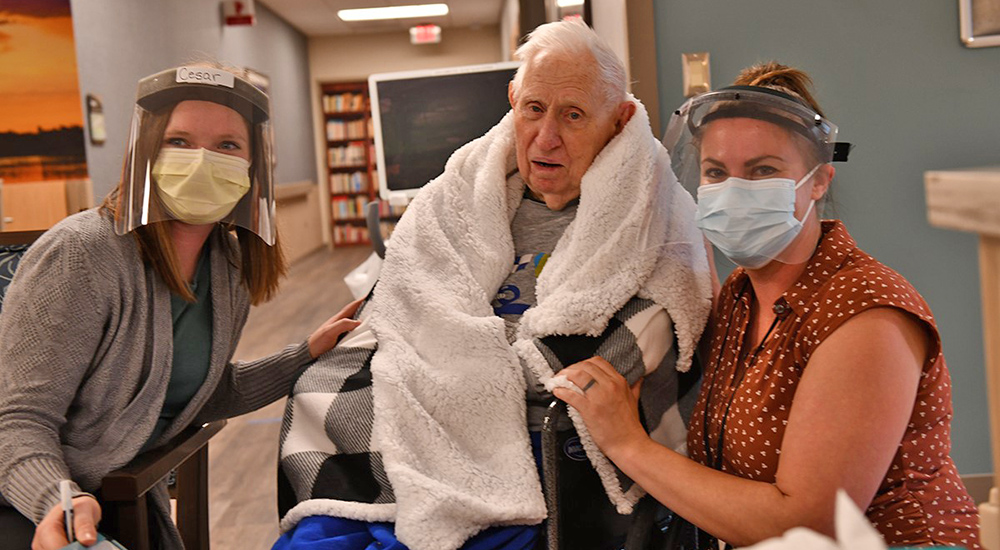
Pictured above, Starks (right) and medical student Amy Parkinson visit with BRO Veteran Richard “Nick” Knickerbocker.
“Generally, unmet needs or stress—such as no longer being able to communicate—causes distress behaviors,” said Starks. “Lots of behaviors are inadvertently caused by caregivers—speaking too fast, using too many words—and Veterans not understanding why, for instance, a stranger is helping them go to the bathroom.”
Feedback from caregivers overwhelmingly positive
As the BRO team learns about the Veteran and finds behavioral interventions that work for that patient, distress behaviors often occur less frequently and may be less severe. This improves quality of life for the Veteran and their caregiver. When the Veteran is ready to return home or be discharged to assisted living or a long-term care facility, the BRO team supports the Veteran and the caregivers by sharing the behavior plan and making visits for up to six months.
While BRO Veterans often have a longer length of stay, Starks says the outcomes are worth it because they are more stable when they leave the inpatient unit. She adds the feedback from caregivers is overwhelmingly positive. One of the greatest challenges is the stigma of dementia even within the medical field.
“Dementia is not felt to be a very glamorous field because we don’t have a pill or a surgery that can cure things,” she said.
But as her medical students and residents spend time with the BRO Veterans—an essential component to building the behavioral care plan—they see the human beings behind the disease and find compassion as they provide care.
“That to me is the most important learning objective,” Starks added, “seeing that these are people and not just problems.”
VA salutes Dr. Jamie Starks, VA’s clinical educators and the more than 1,400 educational institutions that partner with VA to train future health professionals.
These academic affiliations, some of which began more than 75 years ago, are coordinated by VA’s Office of Academic Affiliations (OAA). Find out more about VA’s academic mission by watching this video and visiting the Office of Academic Affiliations website.
Topics in this story
More Stories
Study underscores important role COVID vaccination can have in protecting Veterans from infection and reducing long-term health consequences
Columbia VA’s robotic surgery teams completed their 800th robotic surgery and are on schedule to hit 1,000 by the end of the year.
In a decentralized clinical trial, Veterans can participate from their own homes or local VA instead of having to travel to a research site.







Great information and resource.
Many great answers to many question I have at this point in time