A preacher’s wife. A young mother. A soldier. These brave individuals joined a survivors’ panel to share their experiences and recovery stories during a Domestic Violence Awareness and Intimate Partner Violence Awareness summit sponsored by the Veterans Health Care System of the Ozarks.
According to recent studies, one-in-three women and one-in-four men in the general population report experiencing intimate partner violence. In addition, one in five women who experience intimate partner violence threaten, attempt or die by suicide. Related studies suggest Veterans of both sexes are up to twice as likely as non-Veterans to report experiencing intimate partner violence during their lifetimes.
“There were times I just wanted to give up and didn’t care anymore because I was so ashamed. I had guilt and felt so broken and betrayed by ones I loved,” said Tiffany, who was a victim of Military Sexual Trauma (MST) and intimate partner violence while serving in the military. “But I learned from my VA counselors not to judge myself by what someone else did to me. Trauma may happen to you, but it can never define you.”
“Relationships are at the core of everything.”
These distressing facts are why the Veterans Health Care System of the Ozarks and VA’s Suicide Prevention Office recently collaborated with several community partners on an initiative to educate and support both the survivors and perpetrators of this type of trauma.
“Relationships are at the core of everything,” said Andrea Predl, Intimate Partner Violence Assistance Program coordinator. “Intimate partner violence can be different for different people. It can be verbal or psychological aggression, physical or sexual violence. It can also involve excessive control, coercion or stalking between former or current intimate partners.”
Pictured above, Predl (left) led a survivors’ panel sharing experiences and recovery stories during the Domestic Violence Awareness and Intimate Partner Violence Awareness summit.
Every VAMC has an Intimate Partner Violence Assistance program or coordinator
During Domestic Violence Awareness and Intimate Partner Violence Awareness Month, the Veterans Health Care System of the Ozarks held resource fairs, a White Ribbon commitment event and a summit in Fort Smith to bring awareness, education and resources to Veterans, family members and friends. During the summit, Mental health experts, community partners and survivors discussed warning signs, how to get help, available resources and recovery stories.
While intimate partner violence does not always lead to a mental health or substance use, studies have shown that those who experience it and other traumatic events are more likely to develop anxiety, depression, or post-traumatic stress, misuse substances and have thoughts of suicide.
“Every VA medical center has an Intimate Partner Violence Assistance Program or coordinator who ensures that resources and services are available for Veterans and their partners who are impacted by IPV,” Predl said. “Many VA clinicians and staff have received specialized training related to IPV services and interventions, and are responsive and sensitive to Veteran-specific experiences that can negatively affect relationships.”
Finding support, tools and specialty care
A military combat engineer for 14 years, Tiffany contacted VA for health care and found the support, tools and specialty care she needed.
“VA care has drastically changed my life for the better. With programs like this and people on the other side helping you, I felt there was hope for me. For my fellow Veterans, I encourage you to be open-minded and want to change and heal. I am grateful and blessed because of VA. I am a survivor.”
If you are dealing with MST or intimate partner violence, talk to a VA social worker or health care provider, or call the National Domestic Violence Hotline at 1−800−799−7233 (SAFE) or TTY 1−800−787−3224.
Find more information, resources and VA’s IPVAP Coordinator directory. If you are in immediate danger, call 911 and remove yourselves from the situation if safe to do so.
Topics in this story
More Stories
Bob Jesse Award celebrates the achievements of a VA employee and a team or department that exemplifies innovative practices within VA.
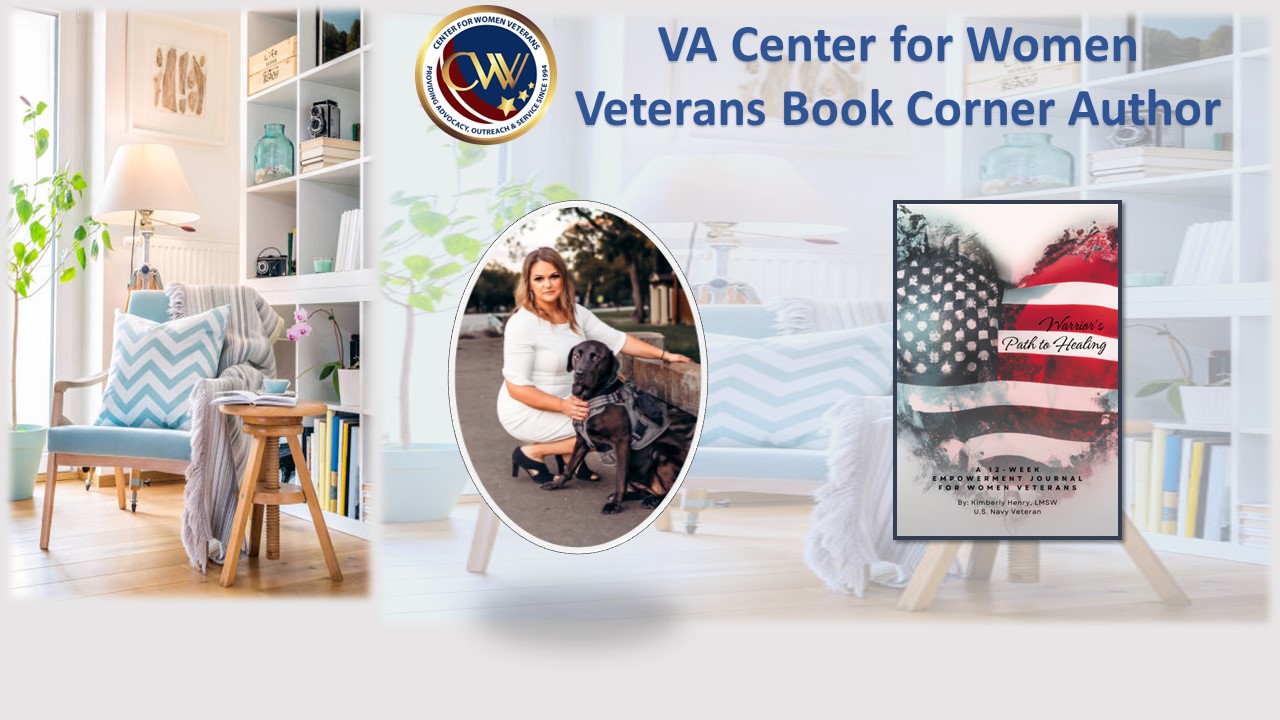
This month's Center for Women Veterans Book Corner author is Navy Veteran Kimberly Henry, who served as a Cryptologic Technician and Sexual Assault Victim Advocate from 2009-2019. She created "Warrior's Path to Healing: A 12-Week Empowerment Journal for Women Veterans."
The Medical Foster Home program offers Veterans an alternative to nursing homes.






the opposite is also an issue. Frozen out of intimacy!
I am a Service Disable Veteran Owned Small Business (medical publishers) for last 33 years, and and we have clinical and forensic references on this subject as will as work book to help with recognition and prevention of violence an abuse against women and children.
Here is my capabilities statement attached https://news.va.gov/126929/different-suffering-intimate-partner-violence/ . I’m confident that I can help, especially knowing the type of medical content we publish.
My name of Glenn Whaley. I can send samples if you want to see our content. Thanks, glenn
I am interested in receiving your sample materials. How do I contact you?