This April, Durham VA was the site of a strategic initiative bringing new hope to Veterans struggling with sleep issues: Virtual Reality (VR) Sleep Quality Improvement pilot.
FireflyVR, a virtual reality software developer, is launching this sleep-focused study in collaboration with VA’s Office of Healthcare Innovation and Learning (OHIL), VHA’s Strategic Initiatives Lab (VA Immersive) and Durham VA.
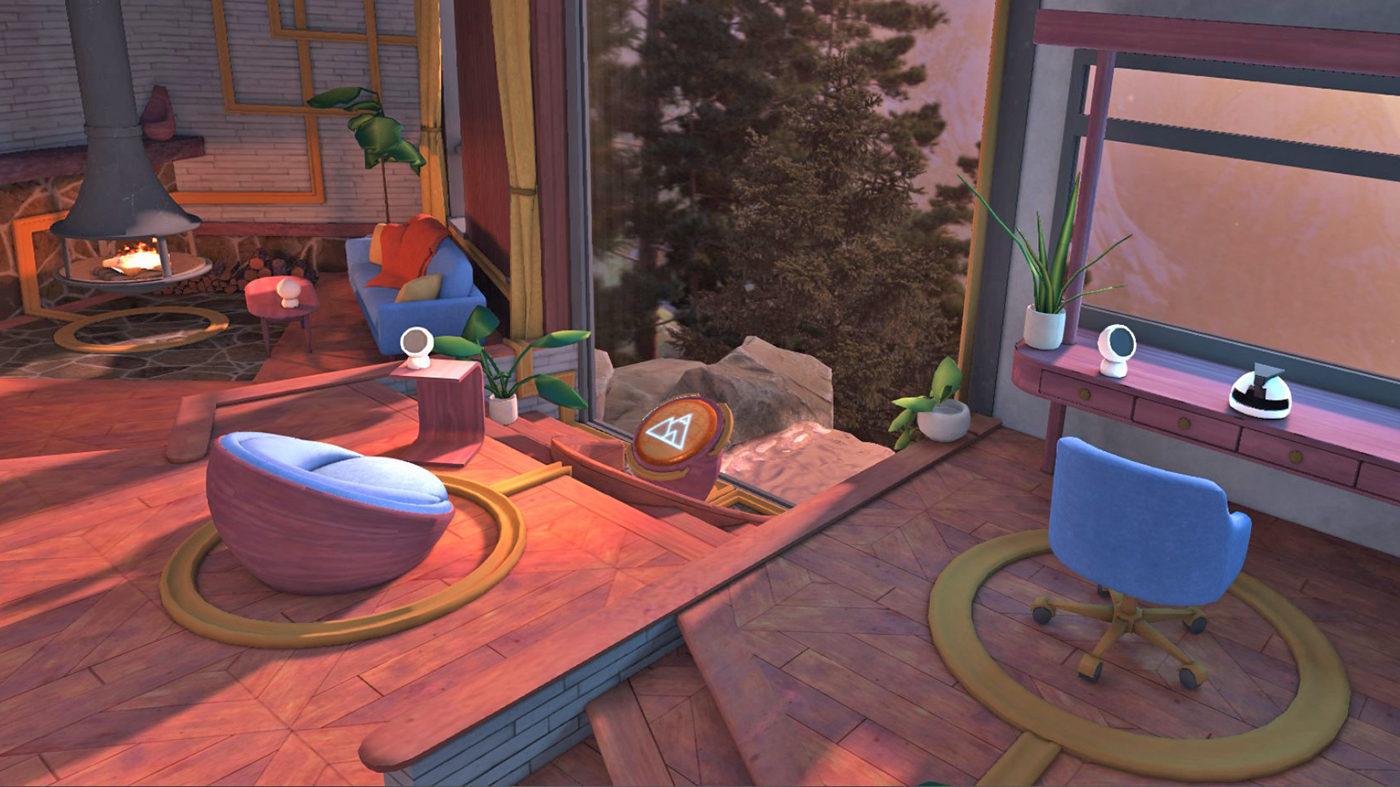
Built on the knowledge of VA’s Dr. Allison Siebern, an expert in sleep disorders, this pilot represents a fusion of VA clinical expertise and innovative technology to elevate sleep health, a crucial aspect of physical and mental well-being. The program features therapeutic visuals through VR headsets, promoting relaxation.
Dedication to Veteran care
The VR Sleep Quality Improvement pilot aims to evaluate and enhance Veterans’ sleep health through targeted VR therapies. “I’m always looking at what innovation we can integrate,” says Siebern. “We want to enhance their treatment experience.”
Outcomes of the initiative will inform the integration of VR into standard care for insomnia, nightmare disorder and positive airway (PAP) acclimation with the potential for broader VR applications.
Siebern honed her expertise at Stanford University’s Sleep Medicine Center and contributed to the development of the Cognitive Behavioral Therapy for Insomnia (CBTi) VA Initiative, which led to VA providers nationally being trained in insomnia treatment. She now brings her extensive experience as a sleep medicine psychologist to the Behavioral Sleep Medicine Clinic with a single goal: improving Veterans’ lives.
Her approach is patient-centric and focuses on non-pharmacological treatments. Veteran care is also personal for Siebern: Her grandfather served in the Army in WWII and her father-in-law served in the Air Force.
Addressing Veteran suicide through better sleep
The initiative aligns with VA’s mission to reduce Veteran suicide, focusing on sleep as an essential component of mental health.
Documented studies highlight the increased risk of suicide attempts, 18 times higher among patients with both insomnia and a mental health condition compared to those without. “Every day in the work we do, suicide prevention is always at the forefront,” Siebern said.
This new program will offer innovative treatments for conditions like insomnia, nightmares and sleep apnea, proactively addressing mental health distress among Veterans and embodying VA’s commitment to effective suicide prevention.
Strategic alliances are driving innovation in health care, offering impactful solutions. This collaboration is a convergence of medical professionals’ expertise, VA’s commitment to care innovation for Veterans, and industry VR technology advances. Their joint effort is focused on creating a VR experience to bring relief to Veterans.
A future defined by innovation and care
As the VR Sleep Quality Improvement initiative takes its first steps, it exemplifies VA’s forward-thinking approach to whole health, using innovation to create new avenues for Veteran care. Led by dedicated VA clinicians like Siebern, this effort also represents the power of collaboration and a deep commitment to the well-being of those who have served.
To find out more about how VA is using VR to innovate, visit the VA Immersive website.
Topics in this story
More Stories
The Medical Foster Home program offers Veterans an alternative to nursing homes.
Watch the Under Secretary for Health and a panel of experts discuss VA Health Connect tele-emergency care.
The 2024 National Veteran Suicide Prevention Annual Report provides the foundation for VA’s suicide prevention programs and initiatives.







SO SAD…BETTER LATE THAN NEVER! QUESTION: WHY…WHY ARE THE VA MEDICAL PROGRAMS ARE SO FAR BEHIND THE CIVILIAN
PROGRAMS ?
WHY DOES THE VA JUST INSISTS IN THROWING MORE “INVESTMENT” INTO ‘INVESTIGATIONS” THAT ARE DUPLICATED IN THE
CIVILIAN MEDICAL LITITURE.. INSTEAD OF PUTTING THE MONEY TO GOOD USE IN VAOPC CLINIC SERVICES AND PROGRAMS?’
IT IS TIME FOR THE VA TO WAKE UP AND START TAKING CARE OF THE VETS WHO DO NOT GET WHAT MEDICAL SERVICES THEY
REALLY NEED AND HAVE BEEN DENIED…LIKE WHY DOES ONLY 70 % OF THE “VETS SURVEYED” CONSIDER THE COMMUNITY
CARE PROGRAM A SUCCESS…QUESTION: WHY NOT TAKE CARE OF THE 30% WHO NEED HELP BUT ARE NOT ADDRESSED
BY THE VA?
Thank you for providing this resource.