Immersive technologies like virtual reality (VR) are becoming increasingly normal health care delivery tools across VA and clinicians are finding new ways to connect Veterans to the soonest and best care.
The VISN 12 Clinical Resource Hub has adopted immersive technology use for its TelePain program led by Specialty Chief Dr. Nadia Hussain and Physical Therapist Shoba Rajamannar-Underhill, who specialize in interventional pain management. The team began prescribing headsets to patients for at-home use and the results have been incredible.
Early adoption and successes
Hussain began incorporating telehealth into her care in January 2023 when she realized it would allow her to connect with her Veteran patients in their own homes. The virtual connection allows her team to provide care to those who may have trouble making it to an in-person appointment, live in rural areas or have anxiety about coming to a facility.
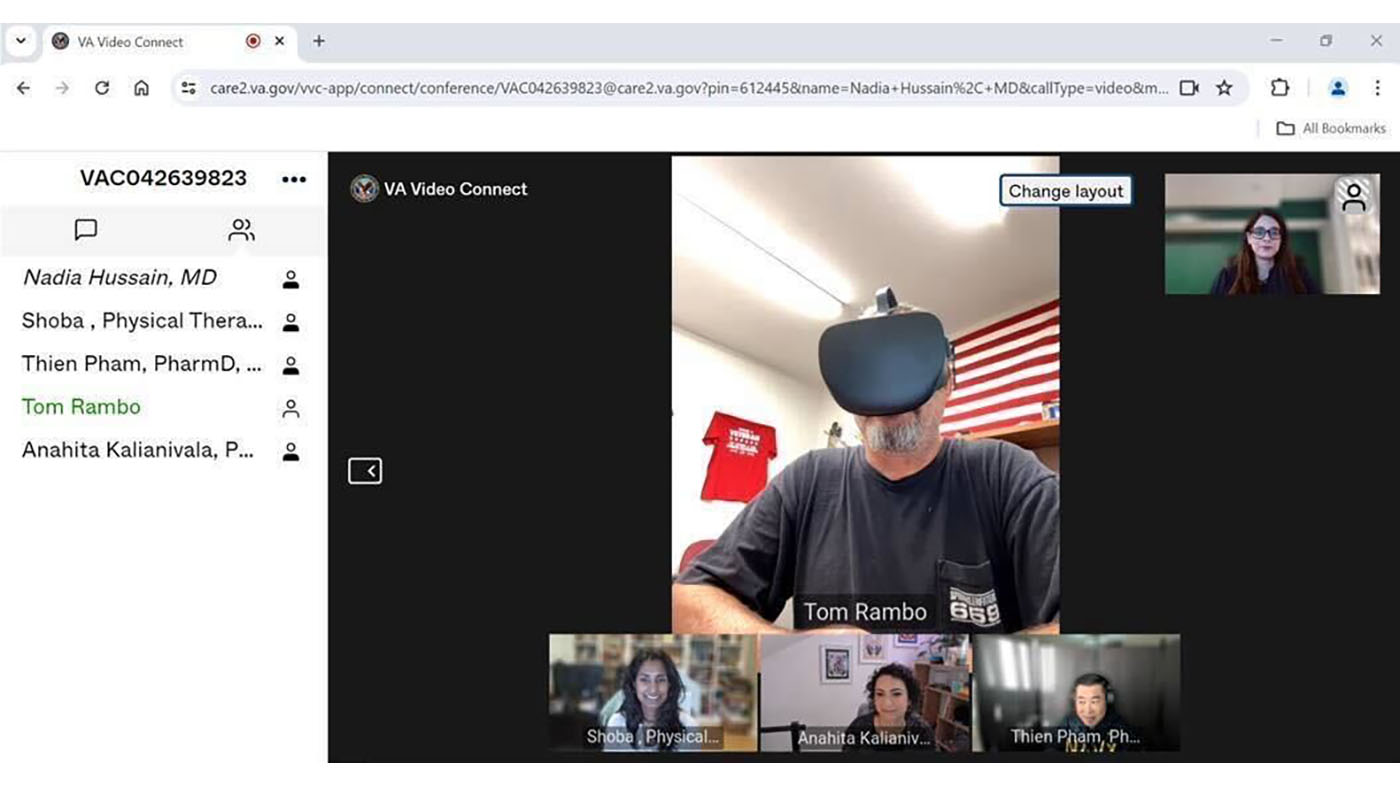
“We are inside their homes as a team. Five of us get in a virtual room and we can see their families, their pets, their lifestyle,” Hussain shared.
Throughout the telehealth process of administering VR, clinicians are with patients every step of the way. They begin with a pre-assessment, monitor progress halfway through and finish with a post-assessment. The team can see exactly how the patients are managing the technology, how much they are being motivated to move and everything in between.
Immersive technology has introduced an effective, manageable way to deliver at-home care. Once the device is prescribed and the trial is completed, it’s shipped to the patient’s home and then shipped back at the end of the eight-week period. Patients don’t need to clean or store devices in between uses and they can achieve results in just a few minutes of daily usage.
Although care is virtual, the connection is real. “They feel supported with our team. We’re engaging them along the way and their mood is better,” said Rajamannar-Underhill. With the incorporation of VR, “All of the Veteran patients have mentioned that they’re able to manage their mood and their stress level, and their sleep has improved.”
One of the methods of measuring uses the Pain, Enjoyment of Life and General Activity (PEG) Scale to assess patient pain interference with daily activities. The TelePain team documented a decrease in PEG scores for every single patient they have followed from beginning to end, indicating decreased pain and increased enjoyment.
Future expansion and collaboration
Hussain and her team are now focused on getting more heads in headsets and increasing utilization of VR in care delivery. Increasing access means increasing the impact and expanding the footprint of care that VA provides Veterans. It’s not just about providing relief in the moment, but also about creating experiences that will stay with the patients for a lifetime.
“You can have the headset for eight weeks, but then the results of it, what you’ve learned from it, those tools are there with you forever,” said Hussain.
The VISN 12 Clinical Resource Hub has recommended immersive technology to over 30 Veterans on behalf of interventional pain management. The team is currently tracking 25 interactions to date, all with reports of decreased depression and anxiety.
Working at VA, especially in interventional pain management, Dr. Hussain said that procedures are selected based upon evidence and what the Veteran truly needs. Immersive technology assists by providing a non-invasive tool for identifying issues and next steps, also serving as a therapeutic escape.
VA Immersive supports more than 2500 VA staff in the exploration and implementation of immersive technology across VA, which has now deployed over 3,300 VR headsets across more than 170 VA medical centers and outpatient clinics in all 50 U.S. states, Puerto Rico, Guam and American Samoa.
To learn more, visit the VA Immersive website.
Topics in this story
More Stories
As severe weather threatened Mississippi, local news warned of a dangerous outbreak of tornadoes. A VA nurse stepped up.
Dorothy “Pat” Rudd, 103, World War II Navy Veteran, has lived a life of service, pioneering the way for women in the military.
VA employees help return WWII items to two brothers’ families. Both brothers were WWII Veterans.





You want people in extreme pain to have a better ATTITUDE! WHAT??? Pain killer NARCOTICS WERE PRESCRIBED TO ME THEN CUT OFF COMPLETELY!!! All other Vets were cut off, too.That was the stupidest thing I have ever encountered in medicine. I/WE NEED NARCOTIC PAIN KILLERS! We aren’t worried about addiction nor are we selling drugs. Pain relief GIVES US A BETTER ATTITUDE. Not some crummy e-game. Lack of PROPER MEDICATION is CAUSING SUICIDES! After we receive medication, THEN we will be happy to play with your toys. YOUR POLICIES ARE KILLING US!!! Please respond!
I’m am a female army gulf war veteran and I am seriously interested in vr and immersible technology. I live in pa and Could you please tell me how to get in touch with someone who could help me? I. Have intolerable pain and I was watching the video on Vr. I’m hoping maybe the va can help with that. Thank you so very much for your time and support