Marine Veteran Jim Warehime survived 24 years in the Marine Corps, including a tour in Vietnam. By early May, he was critically ill with COVID-19, lying in an Intensive Care Unit at the Jack C. Montgomery VA Medical Center in Oklahoma.
Within a few days, Warehime went from bed ridden and near death to discharged thanks to a Mayo Clinic convalescent plasma therapy study.
Warehime’s path to miracle recovery started with a separate event April 24. That’s the date the Eastern Oklahoma VA Health Care System received approval to participate in the experimental study.
That date proved crucial for Warehime. By May 4, the Jack C. Montgomery VA Medical Center staff transferred Warehime, who was critically ill with COVID-19, to the COVID-19 Intensive Care Unit (ICU).
Dr. Kendall Allmaras, hospitalist, registered Warehime in the Mayo Clinic online portal and received plasma from the Oklahoma Blood Institute a few hours later.
“Within a couple of days, he had cleared the infection”
“The patient tested positive upon admission to the hospital,” said Allmaras. “Within a couple days after receiving the (convalescent) plasma, he had cleared the infection. Since that time, he has had two consecutive negative results and was able to be discharged from the COVID unit.”
Ginger Warehime, Jim’s wife for 52 years, called the treatment a miracle.
“He was on his death bed and by the end of the week, after the plasma, he was able to talk and be able to be moved out of ICU and then dismissed from the hospital — all in a week,” she said.
People who have recovered from COVID-19 have antibodies to the disease in their blood. Researchers hope to give convalescent plasma to people with severe COVID-19 to boost their ability to fight the virus.
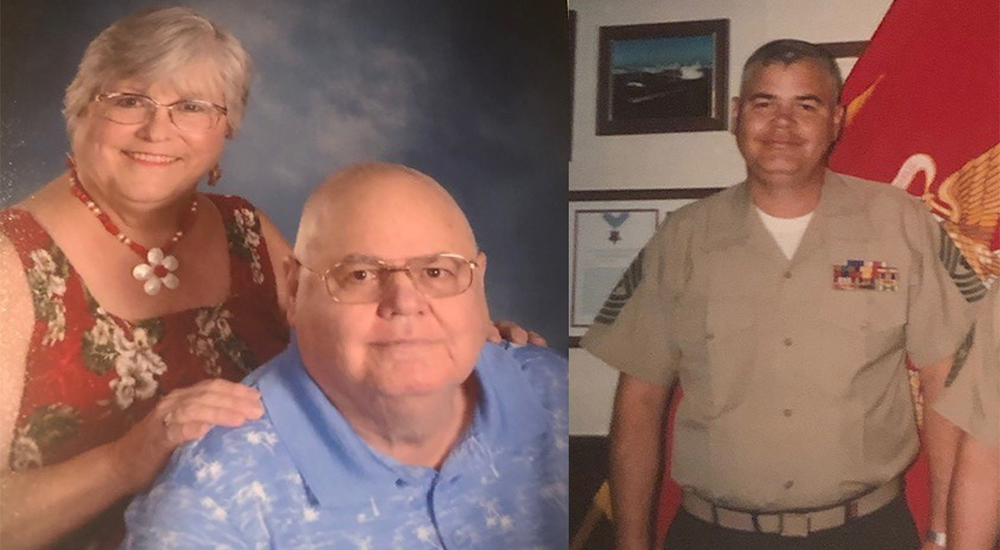
The photo above is Ginger and Jim Warehime who have been married for 52 years. On the right, a photo of Marine Master Gunnery Sgt. Jim Warehime who served 24 years in the Marine Corps and deployed to Vietnam in 1967.
Families are informed every step along the way
Because caregivers and loved ones cannot physically visit Veterans in the COVID-19 units, Allmaras said communication is a vital part of the Veteran’s care.
“We understand that it’s a difficult time for the patients as well as the families,” said Allmaras. “We do everything in our power to make sure the patient is taken care of well and their families are informed every step along the way

Brandon Reich, nursing assistant, and Sandra Staton, RN, with convalescent plasma before administering it to Marine Veteran Jim Warehime
Ginger said not being able to visit her husband took an emotional toll on her, but she is grateful for the compassion the ICU gave her.
“I couldn’t ask for better care,” she said. “I love them all and wish there was something I could do for them because they helped me get through that week.”
Along with telephone calls to communicate with the Veteran’s loved ones or caregiver, the ICU also conducts video FaceTime and Skype calls.
“The patient’s wife hadn’t seen her husband for a long period of time,” she said. “Due to FaceTime, she was actually able to see her husband and speak with him for the first time in a very long time. I think that both uplifted the patient’s spirits as well as his wife’s. It gave her some assurance that things were okay. I thought that was really special and important.”
Once Warehime had beaten COVID-19, Allmaras and the ICU nursing staff shared the news with Ginger.
“I could feel the love and the excitement that they had for us,” said Ginger. “I could just hear it in their voice. It was just so exciting.”
“I just thank God he wanted to go to the VA”
Marie Stanhope, one of the many ICU nurses who cared for Warehime around the clock, said his beating COVID-19 was indeed an exciting moment for the ICU.
“You don’t know until you give it if it’s going to be beneficial or not, because we’ve never had to administer (convalescent plasma therapy) before,” said Stanhope. “Seeing it work was very satisfying for everybody.”
Ginger said she is grateful to VA and the ICU staff who treated her husband.
“When Jim was first diagnosed, he was taken from a skilled nursing facility here in Bartlesville to the ER,” said Ginger. “The doctors asked him where he wanted to go and Jim said absolutely the VA. He wanted to go to Muskogee. I just thank God that he did.”
Warehime thanked the VA staff who cared for him.
“I don’t know what I would do without them,” he said. “They were great.”
Allmaras said the nursing staff and respiratory therapists who provided care for Warehime deserve credit for their work.
“The respiratory therapists were a vital part to our patient’s recovery,” she said. “They spent a great deal of time in the ICU assisting the patient and providing treatment. Everyone tries to go out of their way to do everything they possibly can. They are phenomenal.”
Convalescent Plasma Registry – Help Save Lives!
Nationally, more than 60 VA medical centers, along with the Jack C. Montgomery VA Medical Center, are taking part in the Mayo Clinic study.
“Our facility worked diligently with an interdisciplinary team to get this program approved quickly and to ensure we have treatment options to offer Veterans impacted by COVID-19,” said Dr. Shana Hampton, primary principle investigator for the Eastern Oklahoma VA Health Care System convalescent plasma therapy study. “I’m proud of how our staff has worked together to implement the program”.
Dr. River Smith said while the experimental treatment looks promising, more research is needed. Smith is the coordinator of research and development for the Eastern Oklahoma VA Health Care System.
“In order to do more research, we need to ensure individuals recovering from COVID-19 know how to donate plasma,” she said.
More recovered patients needed to donate their plasma
As the COVID-19 crisis continues, the study needs more recovered patients to donate their plasma.
To provide convalescent plasma, donors must:
- Have a prior diagnosis of COVID-19, documented by a laboratory test.
- Be symptom-free for at least 14 days prior to donation. They also must test negative for COVID-19 (staff will provide testing, if needed).
- Be eligible to donate blood.
Doctors encourage donors to sign up for Oklahoma’s registry at my.bio-linked.org. Bio-Linked allows users to submit confidential health and social information via a secure site. They also can list themselves as potential volunteers for medical research.
For more information, visit https://obi.org/about-us/convalescent-plasma/ or discuss with a primary care physician.
Nate Schaeffer is a public affairs specialist at the Jack C. Montgomery VA Medical Center.
Topics in this story
More Stories
Critical care dosing guides are critical in emergency care where a clinical team’s skill and focus matter most.
Combat Veteran faces the traumatic events of her PTSD during prolonged exposure therapy and looks forward to the days to come.
Bob Jesse Award celebrates the achievements of a VA employee and a team or department that exemplifies innovative practices within VA.