When Navy Veteran Ralph Gervasio Jr. was admitted in the intensive care unit (ICU) at Nashville VA Medical Center in 2017 for acute respiratory failure, he didn’t know that his road to recovery would be one of the most difficult times in his life.
Well into his 60s, the Vietnam War Veteran had maintained a life-long strength and fitness regimen. But after three weeks in the Intensive Care Unit (ICU), Gervasio faced the effects of Post-Intensive Care Syndrome (PICS).
“I can attest to the physical aspect of PICS. I had lost nearly 30 pounds and much of my muscle mass. As a result, I couldn’t curl a 30-pound weight even once.”
Like Gervasio, many critically ill patients experience stressful situations that may cause them to develop problems related to their time in the ICU. It’s a struggle that Kelly Drumright, a clinical nurse leader at the Nashville VA Medical Center, is working to fix.
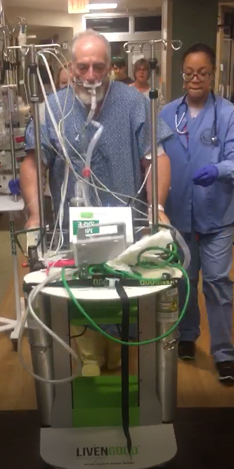
During his stay in the ICU, Gervasio’s care team used ICU Liberation Bundle protocols to help him walk while on a ventilator.
Improving patient outcomes through personalized care
Drumright has 14 years of experience as a critical care nurse. She and her colleagues in VA’s Tennessee Valley Healthcare System implemented a strategy developed with the Society of Critical Care medicine to help Veterans recover from time spent on a ventilator, under sedation, or other treatments associated with ICU care.
This strategy is the ICU Liberation Bundle. The bundle connects processes, people and technology to evaluate a Veterans’ whole health. As a result, their care teams have vital information to provide more holistic treatment, move them off ventilators and transition out of the ICU sooner.
“The Liberation Bundle really creates more of a collaborative team environment in the ICU between the physicians, nurses, the patient’s family, and other providers with the goal of delivering more personalized care,” Drumright said.
Key elements of the ICU Liberation Bundle include:
- Assessing pain using non-verbal cues. Evaluating any disorientation caused by sedation or other medications. Checking for spontaneous awakening or breathing more often.
- Encouraging early mobility and exercise, even for patients on ventilators, to help combat muscle loss and weakness associated with extended periods in a hospital bed.
- Engaging family members in discussions with care teams on a daily basis and organizing support groups for family members and recovery groups for patients to support them during and after their ICU stay.
Keeping an ICU diary helps recovery
The bundle also includes an ICU diary that care teams and families can use to document day-to-day events. It also includes conversations with the patient and what’s going on in the outside world. Keeping a non-clinical record of this information can help patients make sense of memories and confusion associated with PICS. Patients can also continue to add to this diary themselves as they recover.
“At first, I wasn’t aware I had a deficit in this area of recovery. I was no longer a quick-thinker or problem solver,” said Gervasio. “I could not remember what I said a minute removed or even if I had just taken my required meds.
“More than a year later, I still attend my ICU recovery group. I want to give back to those who may need insight to the ICU patient experience. I know I will be giving back for the rest of my second chance life.”
In the photo above, Gervasio stands with his family and ICU care team at the Society of Critical Care Medicine Conference in 2018. While there, he accepted the ICU Hero Award for his remarkable recovery.
Advancing medical care across the country
In 2015, the Nashville VA was one of two VA medical centers selected to be part of the Society of Critical Care Medicine’s 16-month ICU Liberation Collaborative. The collaborative implements the ICU Liberation Bundle at 78 hospitals across the country. The Palo Alto VA Medical Center in California was the other VA facility to participate in the program.
“We once thought a ventilator was the best course of action. Research shows it actually made the patient weaker and prolonged their time in the hospital,” said Kelly. “Using the Liberation bundle, talking with the patient’s family and engaging them in conversations about the patient’s care plan has helped us significantly improve patient outcomes. We have a more complete picture of what the Veteran is going through.”
Drumright is building the ICU Liberation bundle into VA’s new electronic health record system. The system will deploy at VA facilities nationwide over the next several years. Her goal is to help ensure more Veterans benefit from these advancements in ICU care. Her work and that of all the nurses and health care providers who have contributed to the ICU bundle will help improve not only patient’s immediate care in the ICU, but their ongoing physical, social and mental health needs as they recover.
2020 is the Year of the Nurse and Midwife
This blog is part of a VA series recognizing 2020 as the International Year of the Nurse and Midwife. VA salutes the more than 100,000 VA nurses who work tirelessly every day, serving Veterans across the country. VA nurses are committed to taking care of Veterans. As a result, they bring comfort and hope to thousands of patients, 24 hours a day, seven days a week, 365 days a year. We invite you to show your support for these everyday heroes. Thank a nurse at your next telehealth or in-person appointment!
Topics in this story
More Stories
Watch the Under Secretary for Health and a panel of experts discuss VA Health Connect tele-emergency care.
The 2024 National Veteran Suicide Prevention Annual Report provides the foundation for VA’s suicide prevention programs and initiatives.
Theranostics is a specialized field of nuclear medicine that uses a two-pronged approach to diagnose and treat cancer.






