At the onset of the pandemic, VA providers and patients found themselves at increased risk of exposure to COVID-19 due to critical personal protective equipment (PPE) shortages caused by a national supply chain crisis. In response, a team of VA researchers from the Veterans Health Administration’s (VHA’s) Agile Design and Production Transformation (ADAPT) group developed a universal, reusable Powered Air Purifying Respirator (PAPR) hood to protect health care providers from exposure to infectious disease. This innovation is in use at VA hospitals and non-VA medical centers, protecting the lives of frontline health care providers and helping to fulfill VA’s Fourth Mission of supporting the US health care system in times of national emergency.
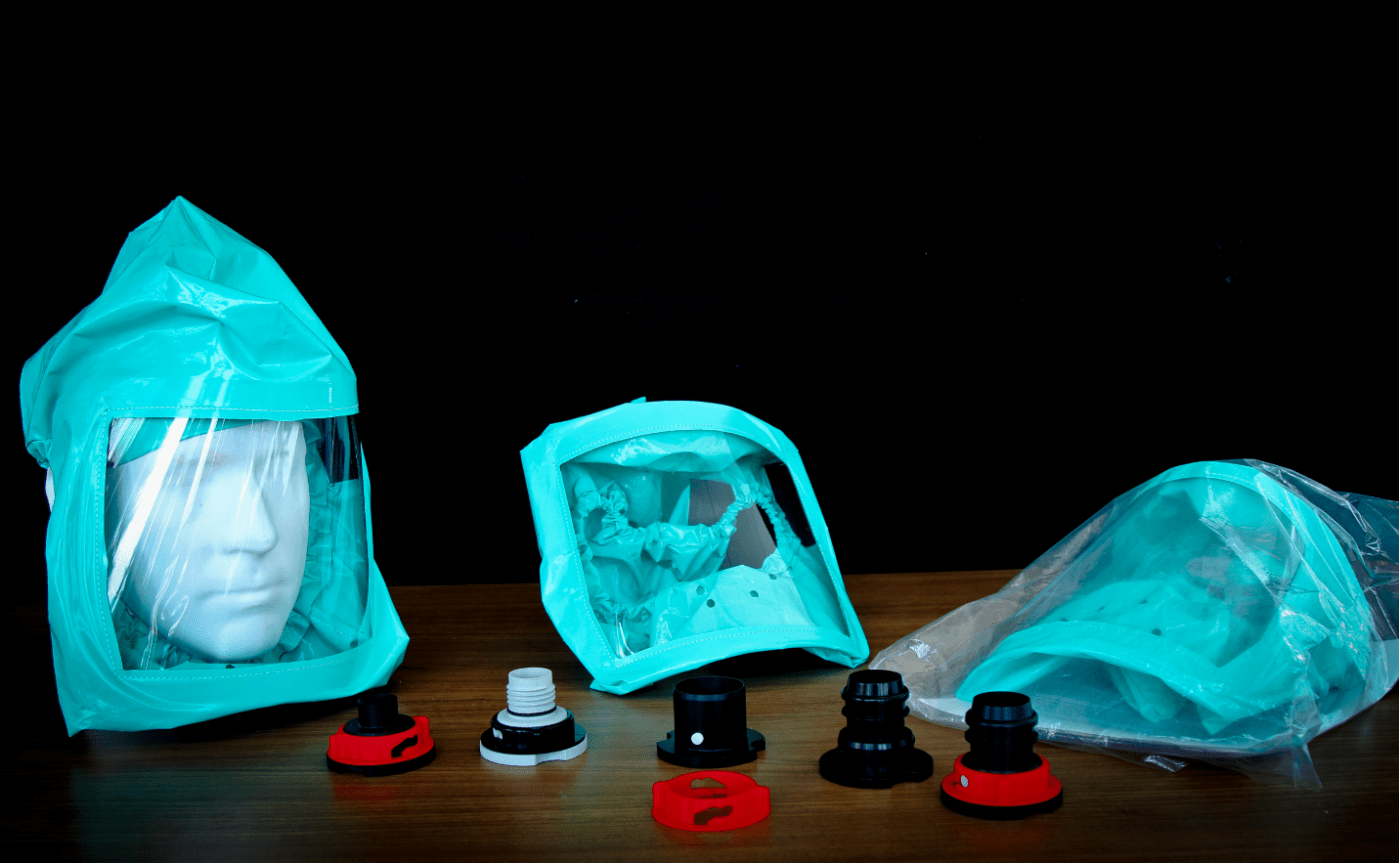
The ADAPT team in Seattle collaborated with Dr. Jennifer DeLaney of Washington University in St. Louis and with Hunter Engineering to leverage VHA’s PAPR hood design in the development of a comprehensive PAPR system. The hood is uniquely interchangeable across multiple types of respirator systems and is designed to improve cleanability during reuse in crisis situations. The National Institute for Occupational Safety and Health (NIOSH) awarded the PAPR hood and respirator system approval for public health emergency use, and the system is listed on the CDC’s certified equipment list.
“Through innovation and collaboration like this, we are having an immediate impact on improving the health and safety of frontline clinicians during the pandemic,” said Beth Ripley, MD, Ph.D., national director of VHA’s 3D Printing Network. “The future of innovation at VA is clear – when the nation is in crisis, VA answers the call.”
This system was developed to be comfortable, reusable and economical. The hood is designed to leave the wearer’s ears free, allowing for easier hearing and stethoscope use, and the large face shield streamlines communication with patients. The CDC rates PAPRs to be 2.5 times more effective at preventing exposure to COVID-19 and other respiratory infections than N-95 masks. Additionally, the masks can be used by providers who cannot wear an N-95 mask due to fit, making PAPRs the clear choice when it comes to safety.
In addition, the PAPR system was designed to accommodate the national supply chain crisis – its materials were chosen to avoid competition with traditional medical textiles and were sourced primarily from US-based manufacturing.
The ADAPT team filed a provisional patent for the PAPR hood and VHA is working with a manufacturer to deliver 6,000 PAPR hoods for local VA use, ensuring continuity of care for Veterans by protecting their frontline providers.
VHA ADAPT was initiated in 2020 to pivot in-house resources, priorities, technology and expertise towards critical health care needs. ADAPT efforts are enabling VHA to rapidly expand enterprise production capabilities to address the shortage of PPE supplies throughout the pandemic, protecting frontline VHA employees and the Veterans they serve.
VHA ADAPT works with VA’s 3D Printing Network to shift in-house 3D printing resources to mission-critical areas during times of crisis. Learn more about VA’s 3D Printing Network here.
Dr. Joseph Iaquinto, is a member of the R&D community at the VA Puget Sound Health Care System, where he applies innovation in science and engineering to overcome the healthcare challenges faced by Veterans and their care providers. He and his co-inventors Arri Willis, Darren Li, and Alex Berardo-Cates, developed the VHA ADAPT PAPR Hood with the support of the VHA Innovation Ecosystem, to aid front-line workers during the COVID-19 pandemic.
Topics in this story
More Stories
Watch the Under Secretary for Health and a panel of experts discuss VA Health Connect tele-emergency care.
The 2024 National Veteran Suicide Prevention Annual Report provides the foundation for VA’s suicide prevention programs and initiatives.
Theranostics is a specialized field of nuclear medicine that uses a two-pronged approach to diagnose and treat cancer.