Over the past few years, VA has been making steady progress to improve how it works with local community providers who deliver care to Veterans on behalf of VA.
Key to this transformation has been VA’s Community Care Network (CCN), both a network and contract vehicle between VA and community providers.
CCN addresses some of the biggest challenges Veterans and providers have had to contend with in the past. Those include referrals, scheduling, care coordination, customer service challenges between VA and Third Party Administrators (TPAs), and claims processing issues.
CCN is making it easier for community providers to give eligible Veterans the care they need while ensuring providers receive timely reimbursement for their services.
What is CCN?
CCN isn’t a program. The VA MISSION Act established a new community care program for Veterans, officially known as the Veterans Community Care Program (VCCP), starting in June 2019. VCCP replaced several existing programs with a new one, which allows VA to purchase health care services for Veterans from certain community providers.
Veterans have to meet specific eligibility criteria to receive care through the program. In other words, VCCP is about what is being provided and who is eligible under federal law and regulation.
CCN, on the other hand, refers to the how, and represents VA’s primary network of community providers. CCN is a contract between VA and Third Party Administrators (e.g. Optum and TriWest) who are responsible for building and managing VA’s provider network for Veterans.
If a Veteran needs a particular health care service and they are eligible for community care, they will likely receive care from a provider who is part of CCN. CCN replaces and enhances VA’s Patient-Centered Community Care (PC3) contract. PC3 is phasing out.
So, if you’re a provider and want to deliver care to Veterans paid for by VA, you need to join CCN by contacting the TPA that administers your region of CCN – Optum or TriWest.
How is CCN better?
CCN works better than VA’s previous networks. Here are some examples of what to expect:
- More timely payments. TPAs now have contract requirements with VA to process and reimburse clean claims from providers within 30 days of submission.
- Prescriptions are easier. Community providers can prescribe immediate-need prescriptions for up to a 14-day supply of medication. More than 59,000 in-network pharmacies can fill the prescriptions.
- CCN offers more services. More types of service providers can participate in CCN. This includes dialysis, comprehensive rehabilitation, residential care, home health care, hospice care, dental, immunizations and long-term acute care. CCN also includes complementary and integrated health services in the areas of biofeedback, hypnotherapy, massage therapy, relaxation techniques and tai chi.
- Simplified appointment scheduling. VA directly manages appointment scheduling for Veterans in most cases. This reduces the number of people a Veteran or provider have to coordinate with.
- Provider-to-provider coordination. CCN has a direct provider-to-provider relationship between VA and community providers. This promotes better care coordination and customer service for Veterans.
Today, CCN delivers most VA community care. This offers community providers a more streamlined, stable relationship with VA when it comes to delivering care to Veterans. And CCN continues to get better as we refine it over time.
CCN Rollout
After more than a year of careful coordination, VA completed the phased implementation of CCN in Regions 1 through 4. All 144 medical centers in these regions are now live with CCN.
TPA Optum manages CCN Regions 1, 2 and 3. TPA TriWest manages CCN Regions 4 and 5. There are 739,475 unique Optum providers enrolled in Regions 1 through 3 and 212,290 unique TriWest providers in Region 4.
Until CCN is fully implemented, Veterans in Regions 5 and 6 will receive health care from their current providers.
If you’re a provider interested in working with VA to care for Veterans, contact the TPA that administers your region of CCN – Optum or TriWest.
Gabrielle Holak and Jonathan Ludwig work in VHA’s Office of Community Care.
Topics in this story
More Stories
Fewer female Veterans were homeless in 2024 than in 2023, but VA is committed to reducing that number to zero.
Keeping Veterans stably housed is one of our top priorities at VA. We have numerous programs to help prevent Veteran homelessness.
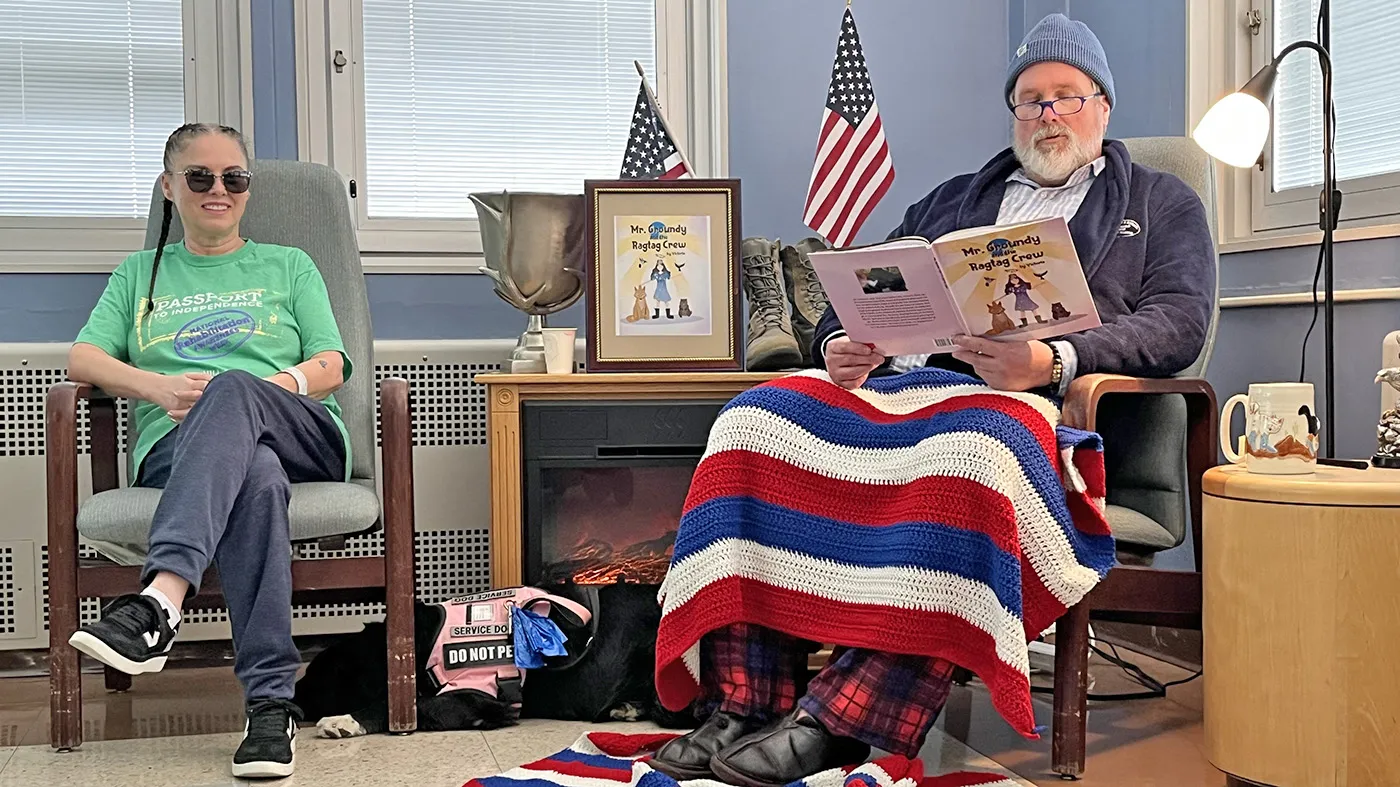
Patients at the Spinal Cord Injury and Disorders Center at Jefferson Barracks VA assembled recently for a very special story hour.