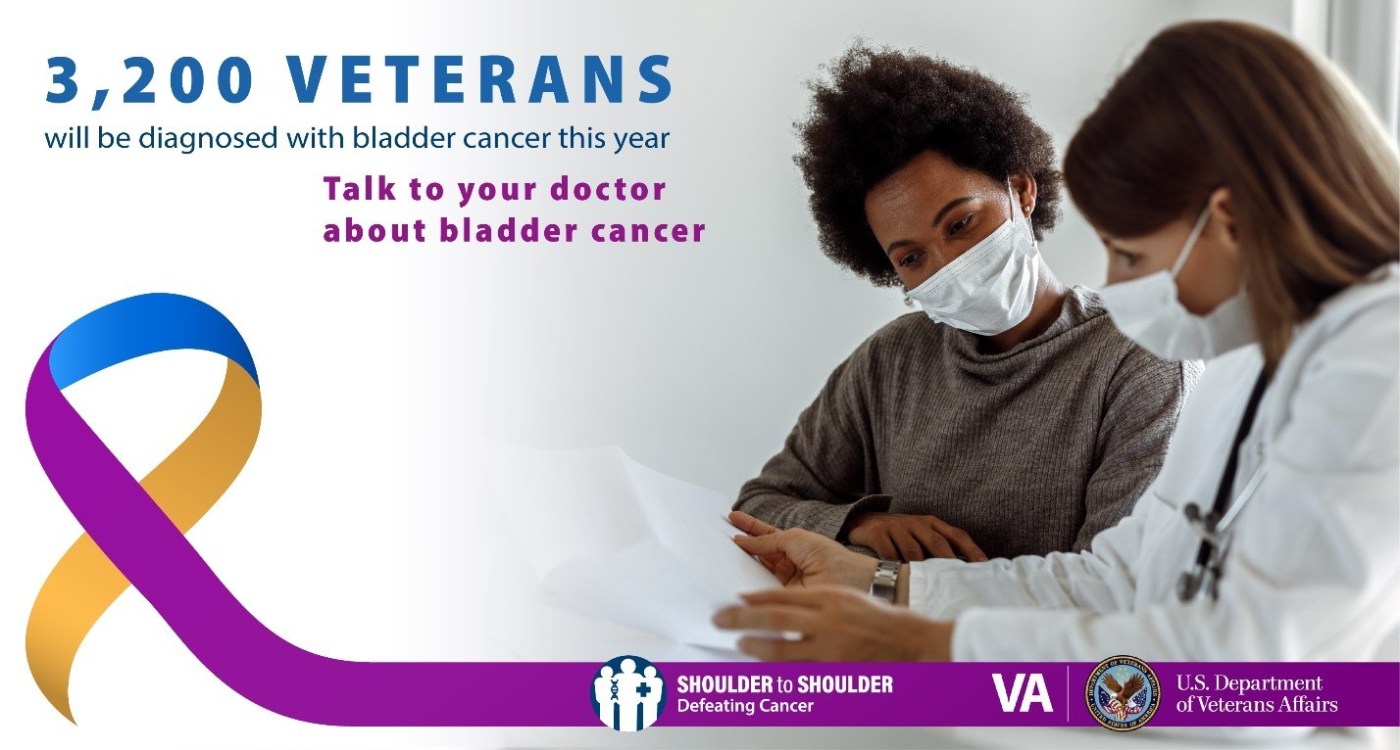
Dennis Roscher served in the Army from 1972-1977 and is one of the 3,200 Veterans diagnosed with bladder cancer each year. Bladder cancer occurs when the cells in the bladder start to grow out of control. Most tumors develop on the inner layer of the bladder, the urothelium. As the cancer grows into deeper layers, it becomes more difficult to treat. Since early diagnosis is critical to successful treatment and recovery, VA is encouraging Veterans to talk to their doctors about the signs and symptoms of bladder cancer.
Bladder cancer is the 4th most common cancer among Veterans. Symptoms of bladder cancer include:
- Blood in the urine; painful or urgent urination; inability to urinate
- Abdominal pain; lower back pain
- Fatigue
- Appetite or weight loss
“Early diagnosis of bladder cancer leads to good outcomes,” said Dr. Chong-Xian Pan of the VA Boston Healthcare System. “Two out of three bladder cancer cases are related to smoking. Even electronic cigarettes are linked to bladder cancer. Quitting smoking is the best way to prevent bladder cancer from occurring.”
According to the Centers for Disease Control and Prevention (CDC), a history of bladder cancer, certain gene mutations, taking some kinds of chemotherapy drugs, and chronic urinary tract infections are risk factors.
Agent Orange and Bladder Cancer
Chemical exposure, such as Agent Orange, also increases a Veteran’s risk of bladder cancer. Thanks to the passage of H.R. 6395, the William M. Thornberry National Defense Authorization Act for Fiscal Year 2021, VA added bladder cancer to its list of presumptive conditions linked with exposure to Agent Orange. Presumptive conditions are certain health problems that are automatically considered by VA to be connected to a Veteran’s military service.
If a Veteran was exposed to Agent Orange in Vietnam and was diagnosed with bladder cancer, they or their survivors can file a VA disability compensation claim at VA.gov. If a claim was previously denied, it will be automatically reviewed. VA encourages Veterans diagnosed with bladder cancer to choose VA, like Roscher, for their cancer care to receive best-in-class treatment.
Bladder Cancer care at VA
VA’s National Oncology Program (NOP) is with cancer patients every step of the way for their treatment. Through the National Precision Oncology Program (NPOP), NOP can identify which cancer treatment strategies will work best for a Veteran’s bladder cancer.
With best-in-class molecular testing through Next-Generation Sequencing (NGS), NOP providers can recommend a course of treatment that targets a tumor’s specific mutation. Pharmacogenomics further tailors a patient’s dosage and options for commonly used medications. NGS enables VA clinicians to leverage the right tools when treating cancer and improve Veterans’ quality of life.
In summer 2021, VA is launching a Clinical Pathways program for bladder cancer. This program will standardize the best practices for bladder cancer diagnosis and care at VA to improve patient outcomes.
Know the signs, seek treatment
Roscher’s healthcare team at the Kansas City VAMC are keeping a close eye on his cancer. Since Roscher noticed the signs and spoke up about them immediately, his doctors caught his cancer very early. The former military policeman encourages all Veterans to see their doctor if they notice symptoms like blood in the urine.
“I know it can be embarrassing to talk about blood in the urine, but just go ahead and do it,” Roscher said. “Use language that you are comfortable with and tell them how it is so you can find out what’s going on. Everyone at VA who I have seen has been genuinely caring. They take the time to listen.”
If you notice any of the signs of bladder cancer, talk to your doctor. Ask your provider to rule out bladder cancer if you see blood while urinating. Identifying bladder cancer signs early is important!
If you are a current smoker, quitting is one of the best ways to reduce your risk of bladder cancer. VA can help. Visit www.mentalhealth.va.gov/quittobacco/howtoquit.asp or call 1-855-QUIT-VET to learn more about smoking cessation at VA.
For more information on how VA works shoulder to shoulder to provide best-in-class cancer care, please visit cancer.va.gov, or contact cancer@va.gov.
Boyd Loehr is a program manager with VA’s National TeleOncology (NTO) program.
Topics in this story
More Stories
Army Veteran Denis Velez donated a painting of his VA hospital as a way of giving back for his treatment there.
Ron Anderson's story of being caregiver for his father in his final years is a journey of love and duty.
Ignoring challenging emotions can negatively impact our health. Breathe through worry, anger and sadness in 5 minutes with this week's #LiveWholeHealth practice.






Hi my name is Theresa Chunko I am a vet. I had contracted Allergic Asthma while serving in the military. I am rated 100 percent Disabled because my asthma is now severe. I getShotseverytwoweeks at the Bay health Medical Hospital.Medicare and Health net pay not through the VA even though it
Is service connected. My Question is is there any kind of help for people who have severe asthma service connected. Because I would like to know if they give grants so people with Asthma can get professional Air purifiers for their home because my Asthma is really
Bad all year long . And I have extreme trouble breathing. Thank you any information or who I ask would be of great helpthe little purifiers I buy at Walmart don’t really work to good that is why I am asking for grants for professional air purifiers to help with my service connected asthma. I am rated at 100 % disabled 100% percent disabled in Delaware SSA thank you the back I go to is in Dover De and the main VA is in Wilmington Delaware. Thank you for your time and assistance Ret USN Corpsman Theresa Chunko
Have you contacted your primary provider (doctor) at VA where you are treated?
I have had prostate cancer( prostate removed ) and I have an appointment with my VA doctor tomorrow. Should I request any tests or exams? Cancer free 4 yrs.