On March 22, 2020, Robert Shaw’s life changed forever.
He began to feel sick in early March 2020. Thinking it was something simple, like a sinus infection, he visited a nearby urgent care physician. He would see a doctor on multiple trips and would receive sinus medication. Unfortunately, this sinus infection just would not go away.
After another visit and more medication, he just couldn’t get his sinuses in check.
Shaw, a Marine Corps and Vietnam Veteran, went to an emergency room and received more sinus medication. He was sure the medicine would work this time, but things took a turn. Later that evening, he started coughing and his wife Valencia called VA for help.
“VA told me to check his temperature to see if he was running a fever, and he was not,” she said. “I was told to keep checking. The next morning, his temperature was 102 degrees. This is when we immediately drove to the Montgomery VA Emergency Room.”
Daughter-in-law died from COVID-19
VA performed several tests and found that Shaw had pneumonia, then admitted him to the Montgomery Campus. Shaw’s COVID-19 test results came back positive, but he was already intubated due to the deterioration of his respiratory status.
The medical team immediately got in touch with Valencia and informed her of the diagnosis. She spoke with her doctors and began her own 14-day quarantine.
The stress hit Valencia hard. COVID-19 was all over the news and began to hit America fast. All she could do was pray. She talked to her church and family members to try to keep it together during those challenging times.
“It was a terrifying moment,” she admitted. “It had really just started, but people were dying. VA doctors were excellent and kept in contact with me every day. They called me to let me know how he was doing – and he wasn’t doing good.”
Valencia would also be diagnosed with COVID-19, along with her son Eric and daughter-in-law.
“My son went to the hospital two or three times,” she said. “His wife was in the ICU. She also was put on a ventilator at Russell Medical Center in Alexander city.”
Shaw’s daughter-in-law would die from COVID-19 complications.
While at the gravesite, Valencia’s phone kept ringing. She initially ignored the calls and tried to focus on saying goodbye to her daughter-in-law. Eventually, she answered, and it was VA.
Robert Shaw was taken off the ventilator. What began as a dark day showed light at the end of the tunnel.
“VA did everything they could and they really care about you.”
After leaving the VA hospital, Shaw went to an acute rehabilitation facility. His doctors were concerned about the blood clots in his lungs. The doctors put him on medication for six months to remedy the issue. However, the effects of COVID-19 didn’t stop there.
“One Sunday, I could tell he wasn’t feeling well,” Valencia said. “The next morning, I took him to the doctor and we found out he had gallbladder problems.”
Shaw spent another week in the hospital. He was still weak from COVID-19 and had to build his strength before surgery. His gallbladder was removed, and he is now paralyzed on one side of his vocal cords.
“I went through a lot,” he said. “There are things I don’t remember. I talked to my pastor before I went on the ventilator and I don’t recall that.”
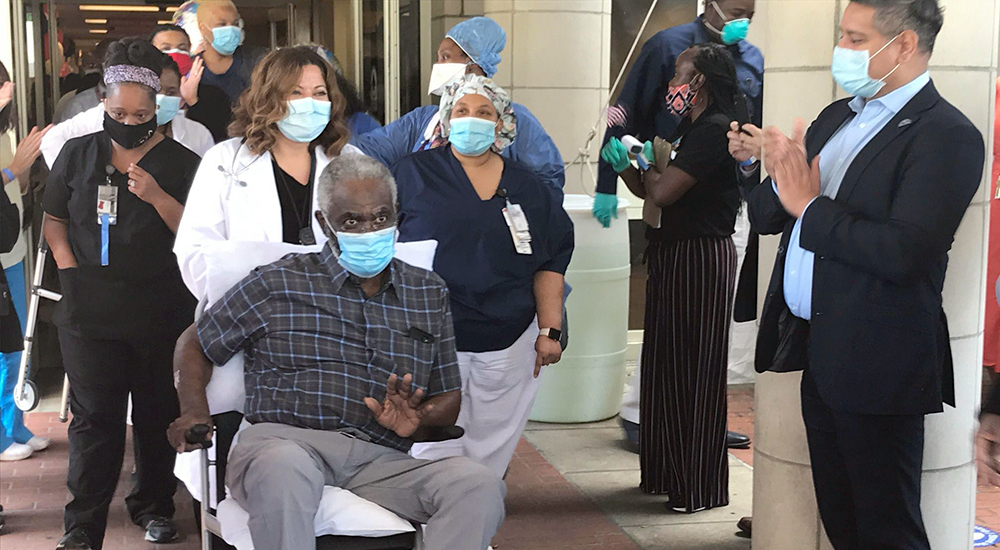
Shaw is thankful to be alive after 20 days on a ventilator, and is very candid about the struggles of the aftermath of dealing with COVID-19. He was discharged on April 30, 2020, after a 40-day hospital stay.
Shaw explained how VA took care of him in the early stages of the COVID-19 pandemic. “They did everything they could and they really care about you,” he said. “I advise people to get the vaccine. You don’t want to go through COVID-19.”
Tramel Garrett is a public affairs specialist for the Central Alabama Health Care System.
Topics in this story
More Stories
The Medical Foster Home program offers Veterans an alternative to nursing homes.
Watch the Under Secretary for Health and a panel of experts discuss VA Health Connect tele-emergency care.
The 2024 National Veteran Suicide Prevention Annual Report provides the foundation for VA’s suicide prevention programs and initiatives.







My daughter caught Covid-19 in December 2020. She was sedated for 2 1/2 months, and had a blood clot in her Aorta (which is very uncommon). She was placed on a ventilator through her trachea. This has caused problems due to scarring in her throat and now she needs surgery to remove the scarring. Altogether she spent 100 days in the hospital and and is currently going through Physical Therapy. She was one of 3 who was as sick as her and she was the only lucky one of the three to survive this virus, Her Doctor calls her “A miracle”. Her Doctor has warned her that she must not catch a cold or get pneumonia as this could cause death. She still has problems with balance and is on the list for a double lung transplant and is now waiting on a donor. Until then she is constantly on oxygen. She will never be the same energetic person that she was and is constantly depressed. Her life will never be the same and I constantly worry that she will decide to give it all up.
And those who think that covid-19 is contained are idiots.
I had Covid last July and pneumonia. I’m glad he’s okay. I’ve had Long Haul Covid for a year now. The VA has given me lots of scans and tests. That’s great. I would like to see the VA take the lead in my home state of WV of establishing the first Covid Clinic for Long Haul veterans. Even civilians. There are none. Many cities now have them. This gives a more concentrated and integrated care. Also docs are on top of research and doing research too. Long Haulers are just left out of much of the Covid medical care. 30 percent of those with covid will develop Long Haul. Many are too disabled to go back to work. There is also a mental component of Long Haul too. It does affect the brain. The Amen Clinic is working with post covid and veterans.
My story is close to the same I’m 79 years old I was was very sick in December my wife tested positive Covid-19 she was omitted to a ICU at a hospital in MADERA Ca my Daughter noticed I was having problems breathing so she took me to the VA ER in Fresno Ca
when I got got there I had 103 temperature with a low O2 and chest pains hard to breathe they started oxygen and took X-ray of my chest and they determine I had double pneumonia in both lungs they also did a Covid-19 test which came back positive started Ivs and 100% oxygen
I also have multiple myeloma cancer
my chance of recovering was very slim after 29 days in ICU I was able to go to rehab I’m still recovering . the VA saved my life I’m so grateful for the Drs and nurse
that took care of me I developed AFIB which the ICU Drs took care of I’m going through physical therapy to regain my strength I want to thank the VA in Fresno for all they did I’m still recovering but better