Leaders of the Million Veteran Program (MVP) are addressing this gap through a new initiative called MVP MIND. It will survey 50,000 new participants with serious mental health conditions about their experiences. MVP officials believe such efforts will lead to more powerful research into these issues and better treatments.
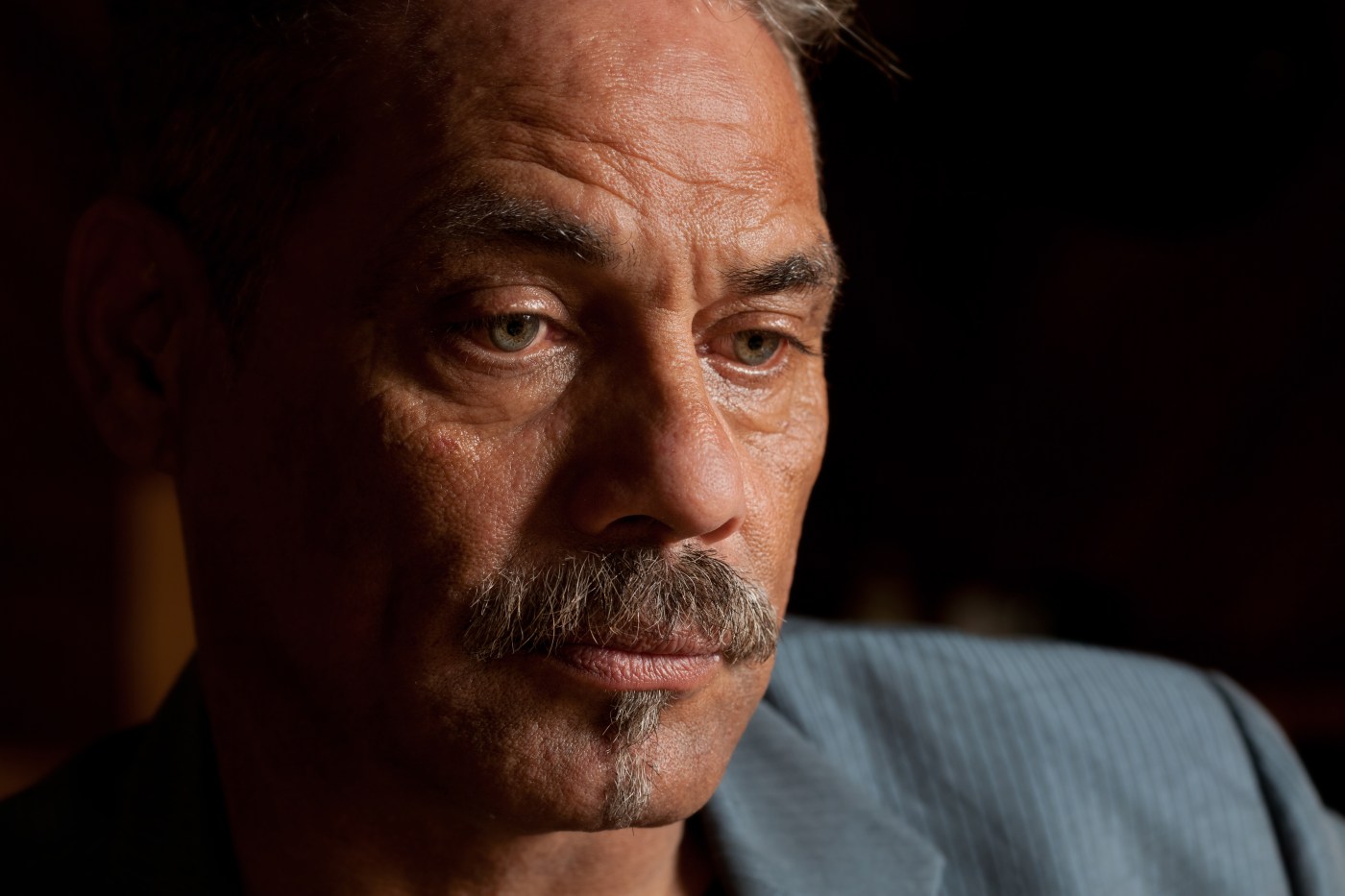
Brandon joined the Marine Corps in 2001 and deployed to Iraq. Like many Veterans, he brought the war home with him. He used alcohol to cope but with help from VA he’s turned his life around.
VA Pittsburgh staff are working to reach more Veterans using mobile mental health apps. Project seeks to increase Veterans’ access to mobile apps to improve mental health coping and reduce suicide risk.
VA will host a virtual career booth at the American Psychiatric Association Annual Meeting, May 1-3 for those interested in a VA psychiatry career.
Established in 2007, Guitars for Vets, a non-profit organization, came together when Marine Corps Veteran Dan Van Buskirk took months of guitar lessons from Patrick Nettesheim. Through their lessons, Van Buskirk was able to learn to play the guitar and since then, the two became friends. Both realized that these lessons created an outlet for expression as well as provided a positive interaction.
However, combat experience was not strongly linked to drinking to cope when the researchers adjusted for a person’s total number of PTSD symptoms.
National Guard Veteran Ken knows VA – he was a doctor there prior to his deployment. When he was injured in Iraq, he skipped private health care, and instead chose to trust his care to VA.
PTSD affects many areas of a woman’s life, including relationships, work, sleep and even reproductive health. Dr. Nillni’s research aims to understand the ways that trauma and PTSD impact women in their childbearing years, and especially during and right after pregnancy. Her research helps women get better care for PTSD during pregnancy, which benefits their families too.
Retired Army Sergeant Major Jason Beighley says leaving the security blanket of the military culture was tough. He shares the three major things he has learned since retiring.
Conversely, the researchers concluded that men with prostate cancer and PTSD may have been at lower risk of death from non-suicidal causes due to favorable physical health resulting from greater health care use and early diagnosis of localized—or low-risk—cancer.
In celebration of Black History Month, VA’s Caregiver Support Program shares the remarkable work of JoAnn Stevens who helps other caregivers and Veterans and shares Black Americans’ legacy.
For mental health providers, understanding cultural impacts and service-related experiences can create a safe environment for assessment and treatment for Vets with PTSD or at high-risk for suicide.