VA’s Office of Connected Care helps Veterans in rural areas receive care through telehealth and other virtual tools.
Home-Based Cardiac and Pulmonary Rehabilitation uses telehealth to eliminate barriers and increase rural Veterans’ access to care.
VA OAA 2022 David M. Worthen Ward recipients are improving care quality, trainee diversity and physician teaching to better serve Veterans.
For Veterans in gender transition, finding their voice can be enhanced with the help of specially trained speech-language pathologists.
The article discussed the results of an earlier study by Kamdar and colleagues that used photo-elicitation to better understand food insecurity in a group of post 9/11 Veterans with children. The researchers found that food insecurity in Veterans is highly intertwined with physical and mental health, military culture, and lack of basic resources like housing or transportation.
Nurse practitioner provides tele-primary care to Native American and rural Veterans in remote areas. “I love being able to impact them.”
More than 500 participants from minority-serving institutions, academic affiliates and professional organizations attended VA’s 2021 Minority Summit to find ways to advance VA academic partnerships and expand diversity in health professions trainees.
VA is committed to providing high-quality health care to Veterans during the coronavirus pandemic and beyond.
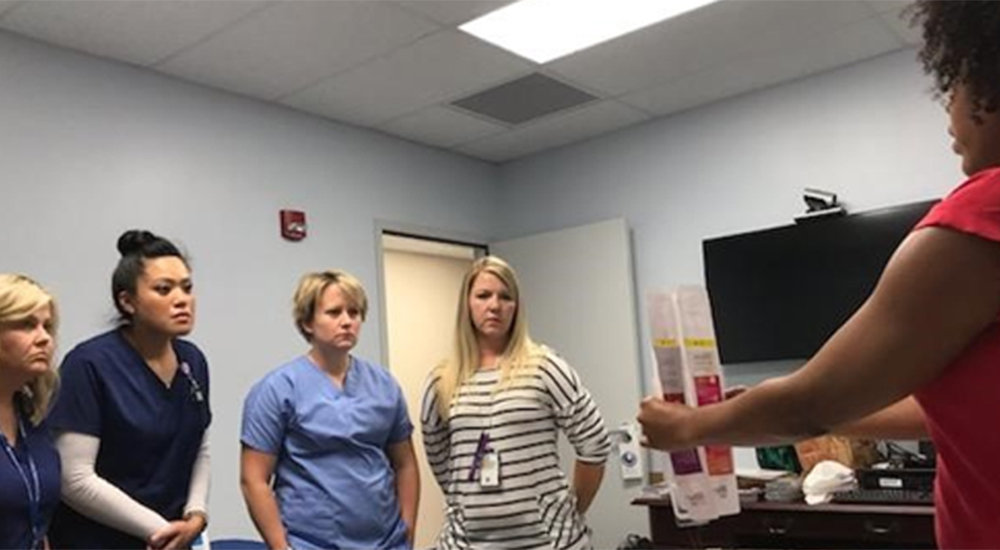
VA provides training on women’s health topics to over 500 rural providers and nurses. Program aims to increase skills related to women’s health. VA is supporting women Veterans in rural communities.
In 2015, VA launched the Technology-based Eye Care Services program. It now serves 22 sites, and researchers are helping to ensure optimal effectiveness.
VA’s Office of Rural Health operates field-based Veterans Rural Health Resource Centers to identify solutions that bring care to where it’s needed most.
VA and SAMHSA host Rural Health Conference to Prevent Veteran Suicide on April 16–17 in Washington, D.C.