Veterans often experience higher levels of stress than the average individual for various reasons. Some Veterans experience stress and anxiety from past events, like combat or a traumatic military training experience. Veterans can also experience stress and anxiety due to reintegrating into civilian life and other life experiences, such as family, work, financial stress and legal matters.
Staff at the Central Arkansas Veterans Healthcare System (CAVHS) recognize how stress impacts daily life and are promoting stress management programs to improve the overall health and well-being of Veterans.
Using feedback to improve the experience
Nakia Williams, Patient Experience program manager, oversees and assists in facilitating Veterans Patient Experience (PX) practices. Williams listens to patients to improve their experience, reviews PX feedback from various data sources, and coordinates improvement efforts and initiatives for CAVHS.
She noticed a downward trend in the overall PX measure for Stress Discussed in the Survey of Healthcare Experiences of Patients (SHEP) survey question, “In the last six months, did you and anyone in this provider’s office talk about things in your life that worry you or cause you stress?”
To improve the measure, she met regularly with primary care nurse managers to discuss stress management tools and resources.
“I realized early on that I could not tackle the measure alone, and it takes a team approach to improve the overall experience,” said Williams.
The team assigned a Stress Discussed Champion, Registered Nurse Cassandra Petersen, to identify the key factors that affected this measure. Petersen then developed the “Stress Less Program” to provide health care professionals with tools for addressing patient stress to enhance their quality of life. She and her team created handouts and flyers explaining stress and how it affects health and information about available programs to improve stress.
“Stress is harmful if we don’t perceive that we have any resources to cope with it,” said Petersen.
They developed a patient stress questionnaire for primary care providers to use during patient visits to assess stress symptoms. The questionnaire asked about feeling worried about health, finances, family issues, and drug and alcohol use. Furthermore, it offers health and wellness programs to reduce stress. Providers could discuss referral options based on the patient questionnaire’s results, such as Primary Care Behavioral Health, Health & Wellness Programs, social work or legal.
“Stress comprehensiveness is what this whole program is about,” said Petersen. “The goal of this program is to improve health outcomes, decrease depression and anxiety, improve sleep, decrease pain, decrease suicide rates and reduce health care costs.”
Integrating Whole Health
As a next step, Williams and Petersen partnered with Whole Health Program Manager Mandia Johnson to integrate Whole Health initiatives into the PX Program.
Whole Health is VA’s approach to care that supports the entire health and well-being of Veterans and employees.
“Whole Health Culture of Care reaches into every facet of VA,” said Johnson. “Here at CAVHS, we started looking past just trying to introduce the bones of the Whole Health Program and started linking it to metrics the facility has targeted for improvement.”
Johnson and her team discussed how Whole Health Culture of Care could address Stress Discussed and other PX measures identified as outliers through SHEP and VA’s Strategic Analytics for Improvement and Learning (SAIL) report. Training, along with a wide range of tools and resources, was provided to clinical care teams to help Veterans live their fullest lives. Whole Health Initiatives included an Introduction to Health and Wellness, focus groups, chaplain services, self-care programs, sleep hygiene, tai chi, yoga, walking groups, financial health, Food & Nutrition and many others.
Enhanced focus on the Health and Wellness consult was included in the Stress Less Program for staff to converse with Veterans and complete a consultation for any skills Veterans would like to learn to help manage their stress.
“It has been a great way to help providers address stress, knowing that many of our Health and Wellness offerings address stress and empower Veterans with self-care tools to improve stress,” said Johnson.
The result speaks for itself
Veterans began to report positive experiences with their care. One Veteran commented:
“During an appointment with my primary care provider, I was intrigued by a questionnaire handed to me by one of my nurses. I am determined to put into practice a couple of the suggested programs, including mindfulness, counseling, and food/nutrition. I believe all three are helping my coping mechanisms.”
After a month of implementing the Stress Less Program, Stress Discussed measures increased significantly. Overall, they improved their scores from 51.9 in Quarter 1 to 62.2 in Quarter 4 of Fiscal Year 2022.
“If you focus on the experience, the measures and scores will improve,” said Williams. “I am blessed to work with individuals that genuinely care about outcomes and are willing to invest in our Veterans.”
Topics in this story
More Stories
Each week, we receive job announcements from employers and employment websites—including RallyPoint, RecruitMilitary, VetJobs and HireMilitary—looking to hire Veterans. This post contains links to job listings for the week of July 22, 2024. Each week, we’ll continue to post relevant and timely listings as we receive them, and for the locations listed.
VA hosted its second virtual regional Veterans Experience Action Center (VEAC) June 11-13 as part of a series targeting recently separated Veterans and military members nearing transition out of the armed services.
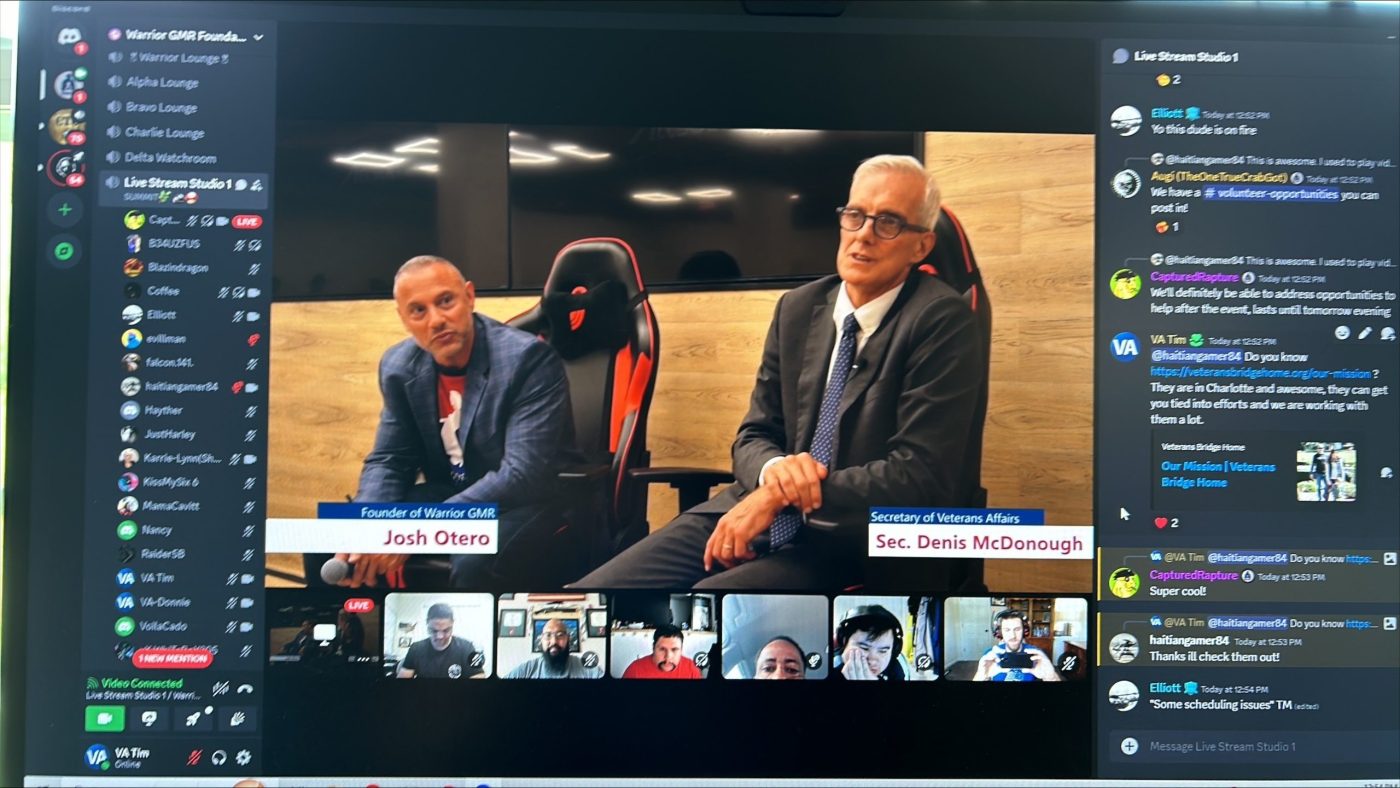
VA Secretary Denis McDonough spoke to Veteran gamers at the Warrior GMR Mental Health and Gaming Summit July 12 in Washington, D.C.






I think the White City, Oregon VA BHIP could benefit from this information. Perhaps sharing is in order?
Hi Susan! Thank you for your comment. I will be sure to share your feedback with them.