Proton pump inhibitors (PPIs) are among the most commonly prescribed medications in VA. Roughly one in six Veterans uses them to ease digestive disorders, such as heartburn or acid reflux. The drugs are effective and well-tolerated when consumed properly.
They are also overused. Studies show that as many as six in 10 PPI prescriptions lack a clear evidence-based indication. Long-term use of the drugs carries a risk of serious side effects, such as pneumonia and bone fractures.
Individual VA pharmacies have been working to lower PPI use for Veterans who do not truly need them. For example, at the Lexington VA Medical Center in Kentucky, pharmacist Kelly Davis says her team’s program has yielded good results.
“The whole facility has bought into it, including our primary care providers. The awareness of the program, coupled with the fact that physicians are seeing more evidence of the risks of long-term PPI therapy, has led providers to be very cautious when prescribing PPIs. As a whole, we’ve found that the program has decreased our unnecessary PPI use.”
National program underway
A national VA program called RaPPID is underway to do the same on a wide scale, and to teach best practices. The acronym stands for the National Randomized Proton Pump Inhibitor De-prescribing program.

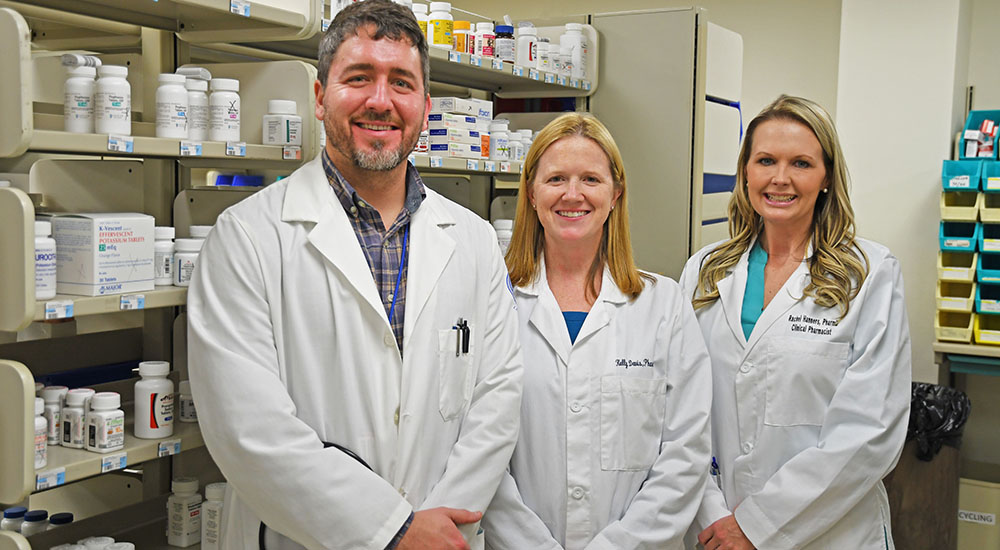
Pharmacist Kelly Davis at the Lexington VA Medical Center in Kentucky has helped lead local efforts to curb inappropriate use of proton pump inhibitors. (Photos by Candace Woods)
The research team is led by Dr. Sameer Saini of the VA Ann Arbor Healthcare System in Michigan, Dr. Loren Laine of the VA Connecticut Healthcare System and Dr. Yu-Xiao Yang of the Corporal Michael J. Crescenz VA Medical Center in Philadelphia.
VA researchers are evaluating the program’s effectiveness. They are working with VA National Pharmacy Benefits Management Services, which is leading RaPPID. The researchers are trying to understand how effective RaPPID has been in improving the use of PPIs and ensuring no negative health consequences, such as peptic ulcer bleeding, have occurred with PPI de-prescribing.
The PPI stewardship team at the Lexington VA (pictured at the top of this blog) has included, from left, internist Dr. Sean Lockwood and pharmacists Kelly Davis and Rachel Hargreaves.
Learning opportunity
“We’re trying to understand the intended and unintended effects of PPIs and ensure that we maximize the learning opportunity for Veterans and the VA health system,” says Saini. “We hope this evaluation will provide not only valuable insight into the benefits and harms of a national effort to appropriately de-prescribe PPIs, but also broader lessons about how to effectively undertake other programs to de-implement low-value clinical practices in the future.”
PPIs account for more than 11 million 30-day prescriptions each year in VA. The drugs are inexpensive on a per-pill basis. However, their widespread use translates into $50 million in VA annually. Current research suggests patients could stop or reduce the use of the drugs in more than one-third of the cases.
Topics in this story
More Stories
Watch the Under Secretary for Health and a panel of experts discuss VA Health Connect tele-emergency care.
The 2024 National Veteran Suicide Prevention Annual Report provides the foundation for VA’s suicide prevention programs and initiatives.
Theranostics is a specialized field of nuclear medicine that uses a two-pronged approach to diagnose and treat cancer.






A local (non-VA) ER physician explained it to me this way. We have bacteria in our stomach. It’s supposed to be there. It helps digest (turn into energy) our food. Our body keeps the bacteria under control by producing acids when necessary. PPI’s severely reduce the amount of acids present. The bacteria grow & grow & grow & grow. There isn’t enough food available to let them do what they’re supposed to do. The bacteria leave the stomach & make you sick. Probably over-simplified but it made sense to me & two days after stopping the PPI (Protonix) I was back to normal. Since then I use Alka-Seltzer or Gaviscon to gently neutralize the excess acids without causing me harm.
By the way, the same ER Physician saved my life once before when he correctly chose between the radiologist on duty & the surgeon who a year before had done his job on me poorly. He recalled the very rare possible outcome of an appendectomy called stump appendicitis. Look it up because if your physician makes the wrong choice, you’re sent home with a PPI & you die.
I use to have Acid indigestion at night for 30 nights straight in my late 20’s. Had a bottle of Malocs on my night stand, which I took every night.. Went to see a family chiropractor, he looked at me, said I had a “curvature of the spine”, which pinched a nerve to my digestive system. He gave me an adjustment, I had no problem that night and a mild case the next night. Went back had another adjustment same thing happen. Because of my job (Plumber a lot of heavy lifting) I’ve seen a family chiropractor (one that uses her hands not a millvolt one)since then. My retired now & I see her every 6 to 8 weeks for an minor adjustment.
Request the mailing address of your FOIA request office to obtain copies of the research papers prepared by Dr. Sameer Saini of the VA Ann Arbor Healthcare System in Michigan, Dr. Loren Laine of the VA Connecticut Healthcare System and Dr. Yu-Xiao Yang of the Corporal Michael J. Crescenz VA Medical Center in Philadelphia since I haven’t located which one of the approximately 400 geographically-dispersed components that may maintain the records I seek.
As appropriate, I plan on filing an FOIA request to get copies of the research papers and then have our friends at Judicial Watch evaluate my findings since, at first glance, the VA doctors appear to have violated Federal law.
MSgt(E-7), USAF (Retired), Administration Superintendent/
Air Traffic Control Operator, 1965-1987, M.Ed.
Vietnam Veteran -100% Disabled (Service-connected)
Presidential Advisory Board Member
The only thing the VA cares about is the almighty dollar, not the veterans. Veterans are only a number to them. I suffer from chronic pain in my back and in my neck (double fracture) and the only pills to ever work was Oxycodone and Hydrocodone instead they put me on Gabapentin which was a waste of time. I ended up throwing the bottle in the doctor’s garbage can. Seems the only way to get the proper medication is to go on the black market and forget the VA to do anything right.
I suffer from severe neuropathy since having my knee replaced (the saphenous nerve was damaged). I cannot even wear a no-show sock on that leg and now I have edema in that leg. The Pain Clinic I’m seen in prescribed for me IV Lidocaine Infusions over narcotics. Let me tell yo that it works, I go every 2 weeks and the treatments last the 2 weeks. Look it up on the internet.
Ask your doctors about this treatment and see if you can get off the narcotics and save some $$$$.
I know your pain. !! The same thing happened to me. I’ve had 7 operations on my back and can hardly walk. They took my painting.meds away and gave me Motrin what a waist of time #! Good luck brother !
No wonder my primary care asked me if I still needed to take them.
I’ve been on PPIs for over fifteen years, For the last five years I was using Rouvastatin. Last fall I developed a chronic cough with a lot of sinus drainage. My ENT tried several different meds including nasal sprays. In early January, I stopped takinfg Rouvastatin, and after five days my coughing stopped, although the sinus drainage did not.
After about two weeks, I contacted my Cardiologist and was advised to take Prevastatin. After about four days my cough returned, this time a little different, but still chronic. I stopped the Prevastatin, but the cough didn’t go away. I believe my cough may be due to acid reflux and sinus combination. I see my ENT in the morning. Have had esophageal dilatation twice.
Due to severe stomach spasms, my Gastroenterologist doubled my dose of omeprazole to 40mgs, which got rid of the spasms, am now back to 20mg’s daily.
I haven’t taken acid reflux pills for 2 years. I chose to stop taking them. I was taking 2 – 20 mg twice/day.
Discovered that I don’t need them. I took them for 6 years until I read the reports about danger of bone fractures.
I have Osteopenia and don’t want to risk it. I think that the pills were, at least, part of the cause.
Thank you for your valuable comments in reference to the VA proton pump inhibitor (PPI) de-prescribing program. I want to reassure all of our Veterans that this program is designed to improve patient outcomes. It focuses on long-term PPI use and asks providers and patients to consider whether a shorter course of PPIs or another treatment should be considered. It also focuses on those who should stay on PPIs to reduce serious health risks, such as GI bleeds. Through surveys, we have learned that patients often stop these drugs themselves even when it is not safe to. Our efforts are driven by the evidence, generated through many studies, about the health risks and benefits of PPIs. In general, research has shown that PPIs can be partially or entirely phased out of treatment plans in many cases without adverse effects to the patient. However, we understand that PPIs are sometimes the only way for patients to control heartburn symptoms and live a high quality of life. The goal of this program is to promote better health and well-being, while reducing the risk of serious side effects in a way that is not a one size fits all. The ultimate decision lies with providers and their patients.
Thanks for the update Mr. Richman, if followed as you describe it makes sense.
I had to endure some serious discomfort but after a month or so I was totally off omaprezole, the serious heartburn issues will fade. My current ENT smiled and shook my hand when I told him I had stopped PPI’s on my own 6 years ago and he had a file of studies on his desk showing the effects of long term usage for anyone to read. My ENT has advised his patients that if they plan to stay permanently on PPI’s find another ENT. Too much data is piling up showing the side effects of long term usage, I don’t think this is just the VA trying to save money.
Here we go, In a “Better for the Veteran” disguise, the VA will, once again, deny veterans much needed medication, solely in an effort to save money. I sure as hell didn’t scrimp on my 30 years of service. I did, however develop Barrett’s Esophagus, a precancerous condition that can easily lead to a couple of different types of cancer. In fact, a good friend of mine and fellow veteran died last year due to esophageal cancer.
What is it the Secretary said in his speech???? Improvements? For whom?
PPIs are awesome but studies are showing associations of earlier death, hip fractures, chronic kidney disease, and dementia in groups of people that have taken PPIs when compared to those who haven’t. I told my VA doc I might as well be dead if I can’t take my protonix. My heartburn is so bad I can’t do anything without it. He agreed I should stay on it. Good to know the info otherwise in 30 years I’d be screaming Why didn’t you tell me?
After many years of using the standard PPI meds, they no longer worked. The past few years I’ve been prescribed Dexilant (dexlansoprazole delayed release capsules) taken once a day just before breakfast…or in my case, the morning coffee. That one little capsule is excellent in preventing GERD and heartburn. If I miss one dose, I’m usually okay providing I don’t eat tomato based foods in the evening. But if I miss two days I’ll get the GERD symptoms with a vengeance.
I don’t use VA services at this time (have never a claim before); I use my employer health care plan doctors. Maybe I’m lucky because private doctors seem more willing to try different approaches to helping their patients than VA doctors.
I use PPI due to reflux induced Asthma. Let’s see where this goes.
Each week we receive an email explaining all the new programs the VA is promoting. Are those programs already funded or are they on the books with no new money? Does the VA need to rob Peter to pay Paul?
Where is the short and long term study to validate the effectiveness of this program regarding the quality of life of veterans who were cut back. Let’s see ALL the data!
I am not a Veteran, but family of several service members and I can assure you from my own experience of all of my teeth decaying, heart valve issues, and my bone density being at the levels of an elderly person at age 28, long term use of PPIs is not a good route. They are trying to prevent more health issues. It doesn’t matter if your heartburn is controlled if it will only end in heart problems, bone and teeth problems, and many more. They also cause the stomach to stop producing the correct amounts of acid. Many times, dietary changes, minor antacids, and stress reduction can help prevent and treat acid reflux. PPIs were never meant to be long-term and there are many lawsuits against the manufacturers from people in their 20s and 30s breaking hips and having heart problems due to anywhere from a few months to a few years on them. The quality of life with those problems is not any better than that of GERD, I can assure you.
I agree with most of these statements. All the V.A. cares about is the almighty dollar and not the veterans they are there to serve and take care of. I was told that I have GERD because I have a hiatus hernia. This is a hernia at the bottom of the esophagus/top of the stomach where the muscle (hiatus) is that opens and closes the top of the stomach. It opens to allow food in and is supposed to stay closed otherwise to prevent stomach acid from going up the esophagus and throat. I can tell you from recent experience that sitting up or standing does NOT prevent the acid from coming up into my throat. It burns and tastes terrible. Most of the time, besides using PPI’s, the recommendation from doctors is to raise the head of the bed to prevent the acid from coming up while sleeping, obviously this won’t work for me when I am getting the acid in my throat while sitting up or standing.
The person who commented on having hernia surgery is correct, the surgery would help. In my case, I have had polyps removed from my vocal cords which may have been caused by the acid coming up into my throat. The other thing that I constantly have is a wheezing when I breath which also my be caused by my reflux. The article regarding Ranitidine and cancer is concerning. I have been put on this medication and it has helped with my reflux, however, I am not thrilled with the possibility of getting cancer caused by the medication that is supposed to help.
When is the FDA going to really do it’s job and vet all these medications thoroughly so that these situations don’t arise? I watch the ads on tv and think to myself, which is worse for me the illness or the cure?
After suffering terrible effects thanks to prolonged PPI use at a young age (had perforated stomach ulcers in high school), I think the fault all lies with the FDA. Anything that cannot make money (actually heals people rather than controlling symptoms) doesn’t get approved and medications like this are not fully vetted and cause problems.I highly recommend looking into some natural options for your hernia and other issues. I found really great relief from some hiatal hernia exercises I found online at my therapists recommendation and they didn’t make my GERD stop, but it is much better than it was. Peppermint tea has helped me, but you can’t lie down after drinking because it relaxed the esophageal muscles. Avoiding acidic foods (citrus, tomatoes, chocolate, coffee, etc) and high fat foods (butter, oils, red meats, egg yolks, whole fat dairy, etc) and adding peppermint, ginger, oatmeal, etc can really help. I’m not a doctor, but I do have a degree in nutrition. I hope this helps you even a bit. I know GERD feels like a catch-22, but my thoughts are with you and your healing.
Of course the true reason here is the way to CUT COSTS.. not to SERVE our veterans? I have to take Protonix twice a day… as prescribed by my outside Gastroenterology Specialist who has been following me for over 20 years. But then again the VA would rather give me a medication that I am allergic to than approve a non-formulary drug too… go figure!
You are going to be at an extremely high risk of osteoporosis. I have personally felt the effects of long-term PPI use and I commend the VA for addressing it. I started Nexium at age 15 for perforated ulcers and ended up with tooth decay, heart problems, and bone density issues. It blocks b vitamins and minerals necessary for bone and heart health from being absorbed and damages your body’s natural acid production processes. Not prescribing PPIs doesn’t cut costs… The pharmaceutical companies will gladly give all their business to the VA. Giving Veterans long-term health issues worse than GERD is not serving them.
I sent Secretary Robert Wilkie a letter VIA USPS.
He didn’t have the common courtesy to respond.
I too have been on PPl’s for most of 30 years. Before that Tums and I were best buds. I am currently on Omeprazole 20mg twice daily. It’s the only thing that works for me. If I miss a dose, I know it right away. Those who have never experienced severe Gerd have no idea how painful it can be. Can’t live without it.
“How to eliminate low value clinical services” …. low value is some value, to some one. But money stopping budget directors and wanna be doctor pharmacists make for a bad gumbo.
Unfortunately I had to go out of the VA system as the VA refused to pay for pantoprazole. It costs more than Omeprazole but is the same thing except with Omeprazole you can’t eat 1/2 hour before you take it or 3-4 hours after you take it. With pantoprazole you can take it before during or after you eat. I found that to be much more convenient as I was often forgetting to take it and end up missing a dose or I would be so busy I’d forget.
I can understand the concern, but the pain is real. If you want to cut down on use of PPI’s what is the alternative treatment?
I have been on these PPI pills for at least 30 something years. I was switched to Ranitidine which led to burning in my throat resulting in a throat scope by a VA MD. This VA Md said Ranitidine was too weak of a PPI med. I went back to Omeprazole. And I am doing good with it.
BUT saving that dollar is like giving faulty ammunition to the troops. Am I really that expensive?
We get it! The bottom line is $$$ and your/the possible kickback. STOP IT! Serve the Veterans and keep it moving. Pills are not always good for our organs or the right fix. The doctor didn’t make the mistake of placing us (a Veterans) on it because it out weighed the side affect(s). This is just another person/group of war room tactics to move care around, funding around, and a name that will hit the highlights saying (I) did this and really you did nothing. Don’t get sick (this team) and run for help and you end up getting the same pill we have then what…you were wrong? Leave GOOD enough alone.
I have been on Proton Inhibitors for nearly three decades. First Prilosec, then Nexium. In 2018 after reading research about the long term affects of these medications, and several hint from my VA primary care doctor, I quit taking them and switched to Zantac 150 which is the same as Ranitidine 150, 2x per day. I had to supplement this with chewable and liquid antacids to maintain, but still had some reflux. At about the five month point I started having problems with my throat and excessive coughing. I made an appointment with my Primary care doctor and I was scheduled for an endoscopy and biopsy. After the procedure I was diagnosed with a stomach ulcer and erosion of my esophagus, and put back on Protonix (Pantoprazole) 40mg, a Proton Inhibitor. Over the next 2 1/2 months, I had to have two more of these procedures, and I was considered healed, and put on 80mg of Protonix, 40mg twice a day. I pretty much can eat what I want, but I have to minimize caffeine so I rink mostly decaf coffee and tea, Sprite, and water, and have been alcohol free for more than 40 years. I retired from the Airforce after 24+ years, so getting the medication from the nearest Base Pharmacy or using Tricare for Life/Medicare.
Time passes, she waits on no one. If the VA is seeing PPI long term usage serious issues developing then I believe it is something to pay attention. I for one have been on or off PPI’s for 25 years. I have had the ultimate surgery to stop GERD, Nissan Funduplication, not fun. What I have found is my GERD is directly connected to the STRESS in my mind. Now that I don’t give a s*** about anything, I can eat my wife’s Spicy Thai food, drink red wine, beer, liquor, eat chocolate, tomato based foods etc. The more I don’t give a s*** the more foods I can enjoy and the less PPI’s I have to consume. Relieve your GERD by not giving a s*** about anything!
Kyle,
Master Diver,
USN (Ret.)
On December 2nd I received a letter that quit taking your identity we will send you something in two weeks this is February 5th and I’m still hasn’t received anything they sent me a pouch to send them back my remaining acid reduction pills I refuse so the VA is going to cut back on using stomach pills acid reflux pills by not just giving them to you so oh well
On December 2nd I received a letter that quit taking your identity we will send you something in two weeks this is February 5th and I’m still hasn’t received anything they sent me a pouch to send them back my remaining acid reduction pills I refuse so the VA is going to cut back on using stomach pills acid reflux pills by not just giving them to you so oh well
I like your attitude. HMCS/USN (Ret)
Why do so many Veterans have GERD and or Barretts Esophagus ? I never had a stomach issue until my service in Vietnam. Over the years I’ve tried all PPI’s that have come out and only Nexium has and is still working. Thus I’ve been on Nexium for decades at levels of up to 4 pills per day and this treatment has been confirmed by many doctors as the most effective treatment for me. Me like others, there is no substitute treatment that I would ever volunteer to do as it’s not worth the daily pain
Stress is the most common cause of acid reflux, so why do you think Veterans have these issues? I was on Nexium from age 15 until I noticed the effects it was having on my teeth, heart, and bones. I have found great natural alternatives in my diet changes, stress reduction/therapy, and a calcium supplement (a form that does not cause kidney stones is key). It’s not quite as effective as the PPIs, but I would never go back after what they did to me and thousands of others I spoke with online.
The statement of how much the VA claims to be paying for these meds, is your reason for them wanting to cut back. It is about the money. Period. I doubt that they care about the suffering, or the damage that stopping taking this medication for those that need it will cause. They took away the pain medications from everyone, because of those that abused it. Now they want to cause more problems by doing this. They do not want to pay for hernia surgery, which could eliminate the need for the acid reflux medicine. I guess the VA thinks that I just enjoy taking it for the heck of it. Believe me I don’t like the fact that I have had to take it long term. I have been telling the doctors for years that I think if they did the hernia surgery, I probably wouldn’t need the medicine. But I suppose they don’t care since it isn’t them.
Would the pharmacist like to be invited to sit in on the Dr.- Veteran appointment so THEY can ensure we get the cheapest and least amount of medication available. I agree with the Mr. Hagen, pharmacist need to get out of the way, do your job and fill the RX as recommended and let the Doc’s do theirs. However, I commend you for hiding the real reason for RaPPID until the last paragraph, however we already know, IT’S ALWAYS ABOUT THE MONEY.
I have been on PPIs for over 20 years due to my severe case of GERD & reflux. I have had three OPEN surgeries to attempt to fix my severe hiatal hernia, w/ very limited success – the first surgery at the old, original Walter Reed Hospital – where an open Belsey Fundiplication was done. Little did I know in a few years that the treatment could be done w/ a scope, vice the scalpel. The only procedure that gave me any relief was the internal Boston Scientific Entryx implant procedure, that effectively builds up your LES & closes the sphincter. It was approved by the FDA, but, no longer, due to some doctors who failed their anatomy class. I’m on MEDICARE & TRICARE for Life. Hope Express Scripts doesn’t get the same idea about PPIs as the VA. The pharmacists are NOT my PCP! But, it’s all about money, I’m sure, at the military veteran’s expense. There will be more cases of cancer if PPIs are taken away.
The only thing the VA cares about is the almighty dollar. Just like the van thief in Albany va. The VA could not care one bit about the veteran, even when it comes to suicide.
All the care about is the almighty buck, no matter how many veterans they screw. Just like the van thief in the Albany va. The last thing the VA cares about is the veteran.
I’ve been using these pills for over 30 years, my doctors haven’t suggested any surgery for my hilatel hernia and then they switched my medicine to ranitidine roughly 4-5 years ago and now I find out that this pill is cancerous, so what is the va doing to help me, I would love to get a reply for this question…..
Beware of the PPI Ranitidine. Google this article on WebMD;
Heartburn Drugs and Cancer: What Are the Risks?
The claim: Ranitidine may be prone to breaking down into a cancer-causing substance. FDA testing found the impurity in generic versions and in brand-name Zantac.
Companies have issued recalls for ranitidine products.
I have GERD
END OF STORY.IF I FORGET TO TAKE MY PILLS I FEEL IT.THEY WORK.
I dont have a “bad” diet. But, if I fail to take my Omeprozole, I’ll have acid reflux, middle of that day. Pop a 1/2 dozen or so Tums, until to take Omeprozole again. I’d rather the VA did not stop providing, but know where I can get the Omeprozole at a “very” reasonable cost
You may be surprised what in your diet can trigger reflux. Fats, acids, salt, etc. Also stress is a huge contributor. I doubt they will stop providing. The article states they want to reduce the use. After personal experience with the effects at a young age, I agree with their choice. Search the effects online and you’ll see thousands of others who have had hip replacements at age 30 and heart issues at age 20… It’s not good and we can thank the FDA for approving them. I’m glad I found dietary changes and exercises that make my GERD very manageable.
Pharmacists should NOT be involved in what a Physicians’ patient is assigned for their given illness. Just stick to reviewing for drug interactions, that’s it; review the script being issued and step aside. This also sounds like insurance providers trying to get in the way to help cut costs. I’ve been taking PPI’s for over 20-years, since 1998; not by choice, but by necessity. Maybe every 2-4 year the insurance company would decide to say no to authorizing my PPI meds, until they receive a letter from the doc saying I’ve tried all the other generics; and I have, I’ve tried everyone out there, only Omeprozole works for my condition. I’ve been examined and scoped several times, and diagnosed with a hiatal hernia where my esophagus meets the stomach. Please don’t mess with what works!!! Thank you,
Bill Hagen could not have stated my case any better, like him, I have been on acid reflux meds for about 20 years and every time my Primary tries to take me off the PPI meds my pain starts and my fight to get the medicine started again is on. I have had no side effects and can enjoy my meals with ease. If these doctors and researchers had our problem they would understand. Like Bill Hagen has said, LEAVE OUR PPI MEDS ALONE.
Bill Hagen could not have stated my case any better, like him, I have been on acid reflux meds for about 20 years and every time my Primary tries to take me off the PPI meds my pain starts and my fight to get the medicine started again is on. I have had no side effects and can enjoy my meals with ease. If these doctors and researchers had our problem they would understand. Like Bill Hagen has said, LEAVE OUR PPI MEDS ALONE.
Don’t you know about prescribing pharmacists?
I have been cut down from a 40mg prilosec to 20mg prilosec and started experiencing severe heartburn on 2 to 3 nights a week. I also have barrett’s esophagus that had started shrinking when I was taking Nexium 40mg. 3 years ago. It is my fear that my condition will worsen without being on Nexium. I now am on prilosec 20mg and famotidine as need.
To me it makes more sense to prevent heartburn all together than to have the need to experience heartburn reflux and allow tissue damage to occur before covering it up with another medication.
I am fearful that I will now develop esophageal cancer and end up costing the VA more to cover my problem with reflux than if I could take the 40mg Nexium that proved to be shrinking my barrett’s esophagus. My civilian gastroenterologist recommends being screened every 3 years which would be this year but my primary VAprovider says 5 years. I HOPE AND PRAY MY BARRETT’S DOES NOT PROGRESS! IF IT DOES IT WILL BE PURE BLATANT NEGLIGENCE!
JULIE SCHEDGICK
I have lots of meds, but I find half a glass of water works fast and effectively
I have a condition called Barrets Ephosegus. My Omeprozole keeps the acid reflux at bay and keeps the condition from getting worse. Do not cut my med back.
I need my acid med please don’t take them away can’t afford in stores
As in my own case, PPIs are usually prescribed to preclude the incidence of esophageal cancer caused by a leaking sphincter. The surgical laser scarring to distort the valve to seal the leakage is not a cure-all and, as-well, an expense that the VA may be unwilling to adopt. I’ll just keep taking the PPIs, as I won’t take the risk of esophageal cancer and the accompanying surgical stoma.
This sounds like pharmacists are trying to get more involved with patient care when they have NO contact with patients whatsoever! Mine regularly mark my script for glucose test strips as “Discontinued” as though my Diabetes is suddenly going to go away. This forces me to regularly ask my PCP to order my next round of test strips, which takes an extra couple weeks. It has now been 19 days since I requested a new supply and I HAVE HEARD NOTHING! Please stay out of my healthcare!
Of course the VA ration’s drugs to Veterans, and seems to be astonishingly skiddish when it comes to pain medications due to the sky is falling reaction of politicians looking for votes. However, let me go to the article, no where did I see any mention of educating Doctors at the VA when it comes to talking with Veterans. We all know, and I’m talking about Veterans, that Doctors at the VA don’t listen, or should I say that very few listen or pay any attention to what we tell them, getting an appointment is like trying to take a hill against adds you know will kill you.
If the veteran is not treated in the VA he goes outside of this appalling system and finds what he needs. So if he has acid refulx he goes to wal mart and buys it off the counter, if what your saying here is that perhaps there is another reason for his issue, then educate the bloody quack to find it.
What it really boils down to is money. That should not be an issue when it comes to veterans.
Interesting article but hopefully the researchers will take into account where there is a familial history of hiatal hernia with accompanying acid reflux before taking individuals off of the PPI’s. Myself, I have switched over to a licorice extract pill twice a day along with using a 150mg ranitidine also twice a day. This regimen has almost completely eliminated my reflux symptoms although the switch over from Prilosec was less than pleasant.
While you’re at it, how about investigating non opioid pain medications for individuals such as myself that are allergic to ALL narcotics because so far I have had 5 open knee surgeries without any real pain medication being made available to me.
I, for one, would love to curb my use of the PPI’s. I have been using them for well over 10 years to treat my GERD symptoms. I have recently been using Apple Cider Vinegar (with “Mother”) and it seems to work well. Just wish that my primary care physician had more time to discuss the matter.
I would help if you actually list the indications & contraindications is laymen’s terms.
You’re rationing at the expense of Veterans. Stop it.