The population of women Veterans is increasing rapidly. In turn, the number of women Veterans receiving VA health care has more than tripled since 2000. This figure has grown from 159,000 in 2000 to more than 510,000 in 2018.
As of May 2017, 26% of enrolled women Veterans lived in rural areas. The demand for comprehensive primary care services for women Veterans is also growing in rural areas. These areas need more primary care providers and nursing staff trained in women’s health.
VA’s Women’s Health Services (WHS) is answering the call. WHS is providing essential resources through one of its newest training programs – the Women’s Health Mini-Residency for Primary Care Rural Providers and Nurses.
WHS and VA’s Office of Rural Health launched this mini-residency training program for rural primary care teams in June 2018. The program aims to increase providers’ and nurses’ skills related to women’s health. In doing so, VA is supporting women Veterans’ long-term health and well-being in rural communities.
Modeled after a WHS three-day training program offered up to twice a year in Florida, the program meets the unique training needs of rural primary care teams. For example, because rural clinics have fewer staff, they may face challenges sending teams off-site for training.
Off-site training can disrupt clinic operations and impact Veterans seeking care. To meet the training needs of rural staff and minimize the impact on patients, WHS is bringing a blended learning training program to rural clinics.
Benefits for women
Participants in the Women’s Health Mini-Residency for Primary Care Rural Providers and Nurses benefit from:
- Online women’s health courses: These explore core topics such as contraception, breast issues and intimate partner violence.
- A one-day, interactive onsite training: This includes case discussions, hands-on simulations, videos of procedures, and exams and live female models.
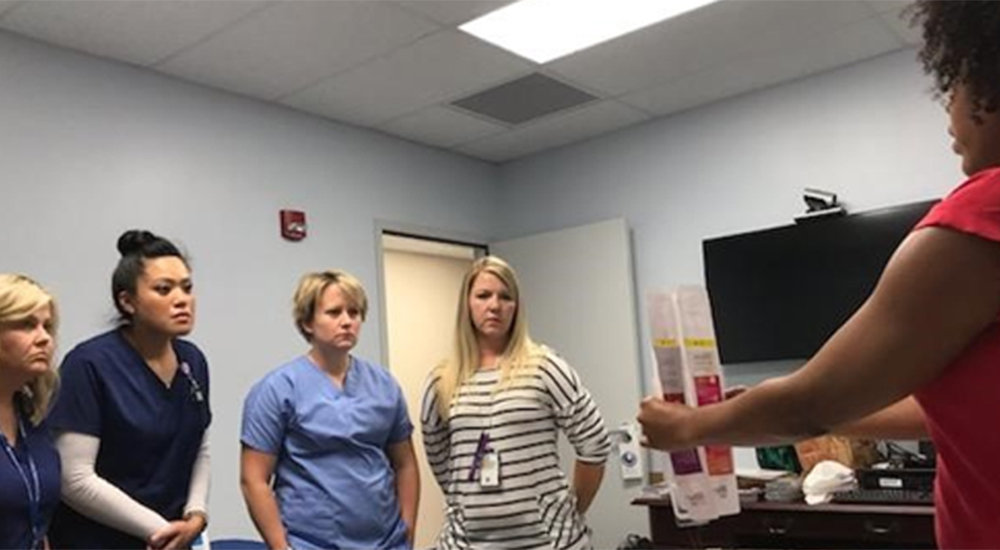
In the photo above, a nurse instructor shows VA nurses at the Murfreesboro, Tenn., VA Medical Center contraceptive options available to women Veterans.
Patient-aligned care team providers and nurses train side-by-side in this program. This aligns with how care is provided. In all, each provider and nurse receive more than 18 hours of accredited medical training.
Since it first launched in June 2018, the program has covered significant ground – from Hawaii to New York and many rural VA sites in between. As of December 2019, WHS has trained 198 primary care providers and 350 nurses during 62 training events. In total, the mini-residency has touched 121 unique VA clinical sites across 24 health care systems.
Highly recommended
This training program has proven effective in improving comfort, knowledge and skills related to women’s health care. In fact, 95% of participants would recommend the training to their colleagues. Feedback from participating nurses and providers includes positive comments, such as:
- “This course was a great learning opportunity. The instructors did very well. I gained confidence to screen and provide care for women Veterans.”
- “I want to say that this was the best interactive course I have participated with the VA in my 29 years of services at VA.”
WHS aims to continue to provide this mini-residency for rural providers and nurses in up to 40 rural clinical sites per year. In doing so, WHS will support the highest level of care for women Veterans in rural areas.
If you have any questions about the Women’s Health Mini-Residency for Rural Providers and Nurses, contact whrmrteam@va.gov. For more information about care for women Veterans, visit https://www.womenshealth.va.gov/.
Aimee Sanders, MD MPH, is a physician educator for Women’s Health Services – Education, Veterans Health Administration.
Topics in this story
More Stories
Watch the Under Secretary for Health and a panel of experts discuss VA Health Connect tele-emergency care.
The 2024 National Veteran Suicide Prevention Annual Report provides the foundation for VA’s suicide prevention programs and initiatives.
Theranostics is a specialized field of nuclear medicine that uses a two-pronged approach to diagnose and treat cancer.






When will Veteran’s Healthcare get out from under Obamacare???
There has been NOTHING kind or nice about the care provided by the VA during this unstable time. They have most certainly contributed to to the volatile situation by their complete apathy and negligent care.
Does the VA need Pharmacy Students willing to work in rual areas, after they obtain their PharmD and pass the national Pharmacy Exam? Is the VA willing to provide a grant or scholarship, workstudy or work aide for attending pharmacy School and getting fully certified? Do they have something like a contract for each year of pharmacy school they pay for the PharmD Doctor pays back two years of working for the VA in a rual area of greatest need. Also six additional months for the VA paying for the Pharmacy Exam? During the summer and Christmas break and on the weekends assign them to get experience at a variety of VA pharmacies. Just trying to help my son out. Any help is appreciated!
This may help.
https://www.vacareers.va.gov/#students
Your response, “Your comment is awaiting moderation” makes no sense. I have no intention of moderating anything I said.
[Editor: That’s an automated holding page telling you that all blog comments are screened and moderated by us, the human, Veteran employees at VA who run this blog.]
Your statement that the “VA is here for women veterans during COVID-19 and beyond” has certainly NOT been my experience. Most assuredly, it has not been here for women veterans who suffer MST, myself included.