Alyssa Knoll, a licensed clinical social worker in the Mental Health Outpatient Clinic at Oscar G. Johnson VA Medical Center, knew she needed assistance with her Veteran.
He stopped wanting to talk during their regular therapy sessions. She had tried several strategies but he was stuck and struggling with thoughts of suicide.
“He didn’t want to live. But he also didn’t want to change or commit to getting better. I didn’t know where to go from there,” Knoll said.
That’s when Knoll remembered a program she had heard about at a Suicide Prevention Coordinator meeting at her facility – the Suicide Risk Management Consultation Program (SRM).

Each consultation has the goal of uncovering what is driving both the risk for suicide and the motivation to continue living for the Veteran.
“I needed someone to listen”
It offers free consultations and training for all providers who are treating Veterans at risk for suicide. Providers can be both in the VA health care system and the community.
As Knoll explained, she felt she had exhausted the tools in her mental health provider toolbox. “I needed another provider’s outside perspective, a strategy recommendation I hadn’t thought of before. What I didn’t realize was that I also needed someone to listen and confirm what I had already been trying.”
Knoll contacted SRM to request a consult and was paired with Dr. Suzanne McGarity. After consulting with Knoll, McGarity realized Knoll’s work with the Veteran was especially complex because there was reluctance to getting better.
McGarity was able to provide Knoll with the support she needed. She approached the issue using a series of suicide prevention tools, including risk assessments and risk mitigation strategies.
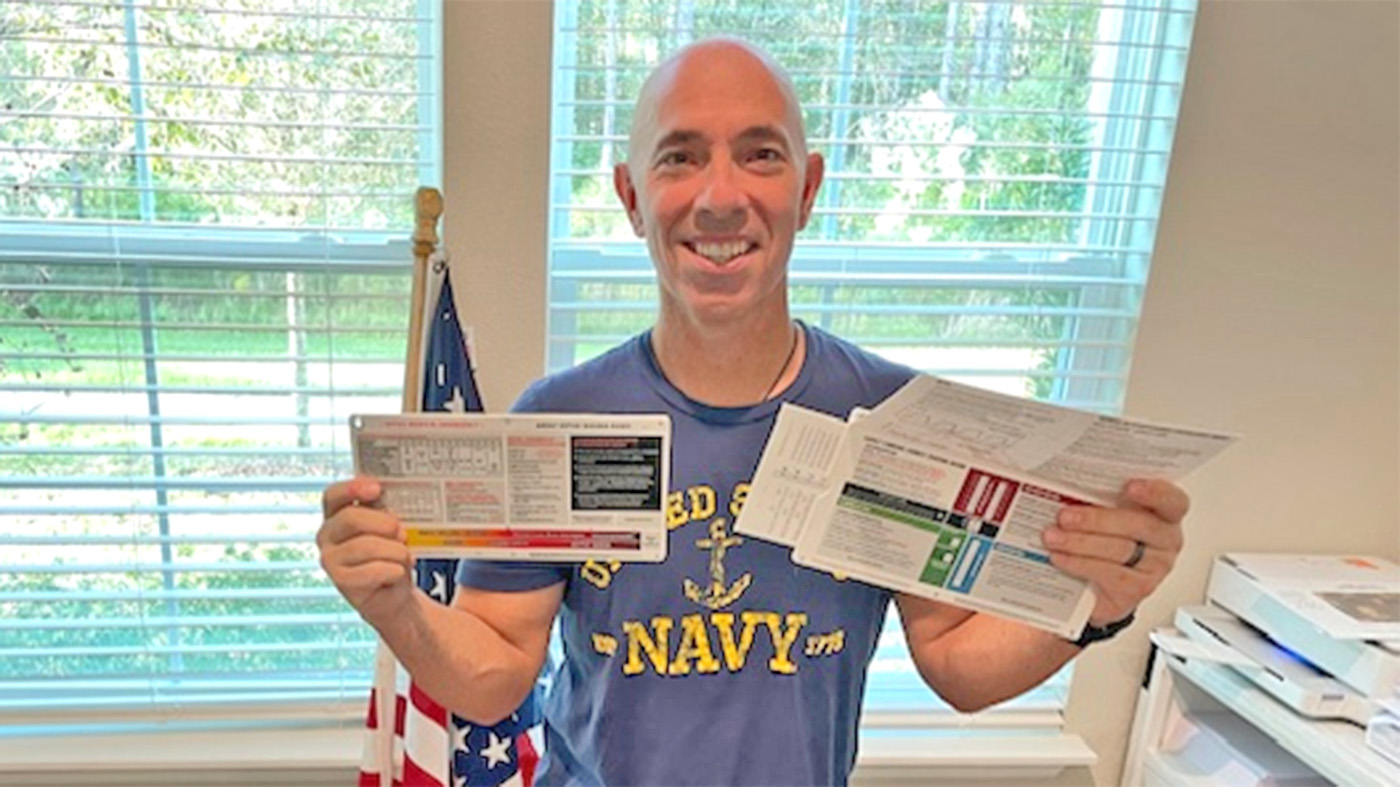
Pictured above, McGarity consults with a provider.
Motivation to continue living
McGarity says she starts each consultation with the goal of uncovering what is driving both the risk for suicide and the motivation to continue living for the Veteran. “We commonly talk about what is driving the long-term, chronic suicide risk for a Veteran.
“Considering suicide is often the result of certain thought patterns, such as when problems feel unsolvable, feeling like a burden to others or that there is little purpose or meaning to life. Risk is elevated when the Veteran’s perception is that the reasons for dying outweigh the reasons for living.
“This is where we, as providers, can help to tip the scale in the other direction. That is when we help the provider working with the Veteran to reduce the reasons for dying and bolster those reasons for living.”
For Knoll, McGarity suggested she use a motivational interviewing tip sheet developed by the SRM program to keep the Veteran focused on doing the work to get better.
“The motivational tip sheet was something I didn’t have in my own toolbox and it was helpful to have new strategies I hadn’t thought of or knew about yet,” Knoll added.
Interpersonal process is invaluable
Knoll continues to work with the Veteran on engagement and says some days are better than others but that having McGarity ask about the interpersonal process between her and the Veteran was invaluable.
“I really was questioning how to help this Veteran. What had worked with others hadn’t helped and I needed new tools to offer. I really didn’t want to lose this Veteran. SRM and Dr. McGarity really validated everything I had already been doing with him to get him better. They made me feel that the anxiety and stress I am feeling about my patient is normal and not because I’m not a good clinician.”
McGarity echoes Knolls’ sentiment about building a provider’s confidence. “Even though I am the consultant during a call, this is a provider to provider relationship and conversation. We have been in the same position, have had similar experiences and can empathize.
“Feeling like they are walking away with concrete mitigation strategies is good, but when they are walking away from the call feeling confident in their work as a provider, that is when I know I have done my job.”
Megan Harvey is the program evaluator for the Suicide Risk Management Consultation Program. She is a licensed psychologist and a prior Local Practice and Recovery coordinator. Gina Pattison is a health writer supporting communications for the Suicide Risk Management Consultation Program.
Topics in this story
More Stories
Forget 'No Pain, No Gain'—try 'No Pain, More Gain' with Tai Chi! Calm the mind and gift yourself well-being in this week's #LiveWholeHealth practice.
Critical care dosing guides are critical in emergency care where a clinical team’s skill and focus matter most.
Combat Veteran faces the traumatic events of her PTSD during prolonged exposure therapy and looks forward to the days to come.