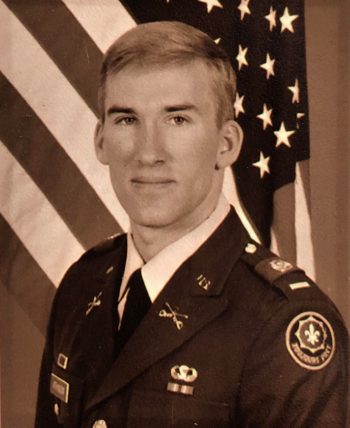
Thirty years ago this month, David Atkinson was part of a cavalry regiment immersed in a ground offensive in Operation Desert Storm. The Army unit headed north from Saudi Arabia into Iraq, then moved into northern Kuwait and engaged Iraqi Republican Guard forces, driving them back into southern Iraq.
During the ground offensive and in the ensuing months, Atkinson and his comrades were exposed to many burning oil fires that Iraqi forces set during their retreat.
“The fires filled the skies with smoke and soot that we breathed in daily,” Atkinson remembers.
Today at age 56, Atkinson is fighting another battle – this time a case of aggressive prostate cancer. Thanks to treatment at the VA Portland Health Care System, his condition has improved dramatically in recent months through precision oncology – the molecular profiling of tumors to identify targetable alterations that can be treated therapeutically. Most recently, his PSA level had plummeted to 0.2, after a high of 115 in December.
The PSA (prostate specific antigen) score is the main screening tool for prostate cancer.
First time using VA
This is Atkinson’s first go-round in the VA health care system. For nearly three decades since his departure from the Army, he found no need to use VA services. He’s discovered it’s never too late.
“I always knew [VA services] were out there,” he says. “But prior to my cancer diagnosis, I was always extremely healthy. Literally, I’d see a doctor once every 10 years… for a checkup at the ages of 30, 40, 50. So I never had a need or a reason to use VA services because I’ve never had anything other than a normal doctor checkup for years, which my insurance covers no problem.”
This time, there was a problem.
Last year, Atkinson’s private health insurance company twice denied him coverage of the immunotherapy drug pembrolizumab, which had been prescribed by an oncologist at Oregon Health & Science University, Dr. Julie Graff. In immunotherapy, a form of precision oncology, organisms in the body’s immune system are used to fight cancer.
`VA being so mission-driven’
Graff, who is also the section chief of hematology and oncology at VA Portland, thus took steps to get him enrolled at that VA facility so he could be treated with pembrolizumab without any potential resistance. He enrolled on Nov. 19 and began treatment two weeks later. He has since received five shots of pembrolizumab, one every three weeks, leading to the promising results he has seen thus far.
In Graff’s opinion, VA’s ability to enroll Atkinson and immediately get him the cancer treatment he needs exemplifies how the agency does “incredible things for our Veterans.”
“VA being so mission-driven to help Veterans really served David well,” she says. “We are taking more patients from outside VA who may be eligible for benefits and getting them enrolled quickly, specifically when they have cancer. David benefited from that. I wasn’t getting anywhere with his insurance company. He may never have gotten the immunotherapy if he weren’t a Veteran. I struggle with that with other patients who aren’t Veterans. Sometimes, I just can’t get them their drugs.”
`The outcome doesn’t matter’
In VA, prostate cancer is one of the most commonly diagnosed forms of cancer among Veterans, many of whom also have service-related exposure to carcinogens. Prostate cancer is most common in men ages 65 and older. The disease is usually found in its early stages and often grows slowly. Most men live with the cancer for decades without symptoms and die of other causes even without early surgery.
Precision oncology is fast developing and has entered the mainstream of clinical practice, with application to a myriad of cancers. Each cancer patient may have different mutations in play, and researchers are learning how to leverage this genetic information to improve outcomes. Immunotherapy, chemotherapy and targeted therapy, all of which are used to kill aggressive cancers that have spread in the body, are forms of precision oncology.
Atkinson, a 1987 West Point graduate, was in the Army from 1987 to 1992 and reached the rank of captain. Despite his health challenges of today, he does not regret having served in the U.S. military.
“I am proud to have served my country,” he says. “The outcome doesn’t matter.”
More information
Click here to read the full story and sidebar.
Click here to learn more about VA research.
Topics in this story
More Stories
In a new series that highlights advancements in VA health care, VA researchers and clinicians are appearing on a Veteran-themed media platform—Wreaths Across America Radio—to tout their critical work.
Recently published findings from the VA Disrupted Care National Project [...]
Diverse representation of women in health care research allows MVP to make discoveries for women’s health