The Career Development Program of VA’s Office of Research and Development provides mentoring for junior researchers so they can learn from experienced VA researchers. Graduates of the program have become national and international leaders in their fields.
We interviewed Career Development awardee Dr. Miranda Lim of the VA Portland Health Care System in Oregon about her research on sleep problems affecting Veterans.
What do you study?
I am a neurologist who specializes in treating sleep disorders. My research program, Sleep & Health Applied Research Program (SHARP), aims to understand sleep and the impact that poor sleep can have on the brain and body.
I study how sleep is affected by common conditions among Veterans, including traumatic brain injury (TBI), posttraumatic stress disorder (PTSD), Parkinson’s disease and Alzheimer’s disease
How did you first get interested in this topic
I decided to become a neurologist because I have always been fascinated by the brain, brain health, aging and human behavior. Sleep is one of biology’s greatest mysteries. We still don’t know why we need to sleep. Understanding how sleep needs might change over the lifespan and in certain medical conditions is the crux to understanding healthy development and aging
What attracted you to VA?
I have had the privilege of serving our nation’s Veterans at multiple VA hospitals around the country. This started with my medical training over 20 years ago. I am grateful for the opportunity to give back to those who so generously gave for us in defense of our country. I cherish the connections that I’ve made over the years with my patients.
VA has built an incredible, unparalleled nationwide infrastructure that cannot be matched by any other health system in the U.S. In the clinical sleep world, we are on the cutting edge of telehealth and the latest equipment for sleep apnea.
In the sleep research world, we have discovered unique sleep disorders tied to TBI and PTSD, allowing us to forge new understanding of how the brain works and new treatments for sleep problems.
Why is your work important to Veterans?
My research particularly benefits Veterans because they are disproportionately affected by TBI and PTSD – both of which can cause sleep problems. For example, my team recently discovered that Veterans who are diagnosed with a TBI or PTSD are at greater risk for rapid eye movement (REM) sleep behavior disorder (RBD), which causes violent movement during the REM stage of sleep.
RBD has been linked to the development of Parkinson’s disease. However, we still don’t know whether Veterans with RBD are also at higher risk of Parkinson’s disease – and if so, how might TBI/PTSD trigger this neurodegeneration? These are incredibly important questions that need to be answered for the sake of understanding what our Veterans are going through.
What do you do outside of work?
I live and breathe sleep research and I love working with my incredible research team. It’s sometimes very hard for me to step away. But, I do have a life outside of research.
A little-known fact about my distant past: I played division I women’s water polo. It was at the University of Southern California from 1994 to 1998. Currently, I love spending time with my family, including my incredibly supportive husband and our three young children.
My older two children have a diagnosis of autism spectrum disorder. It has been an amazing journey that I am grateful to share with them. I’ve learned to understand the world through their eyes – they teach me so much every day.
We love to hike and camp and learn all about native plants of the Pacific Northwest. Our favorite place to camp is in the Olympic National Forest.
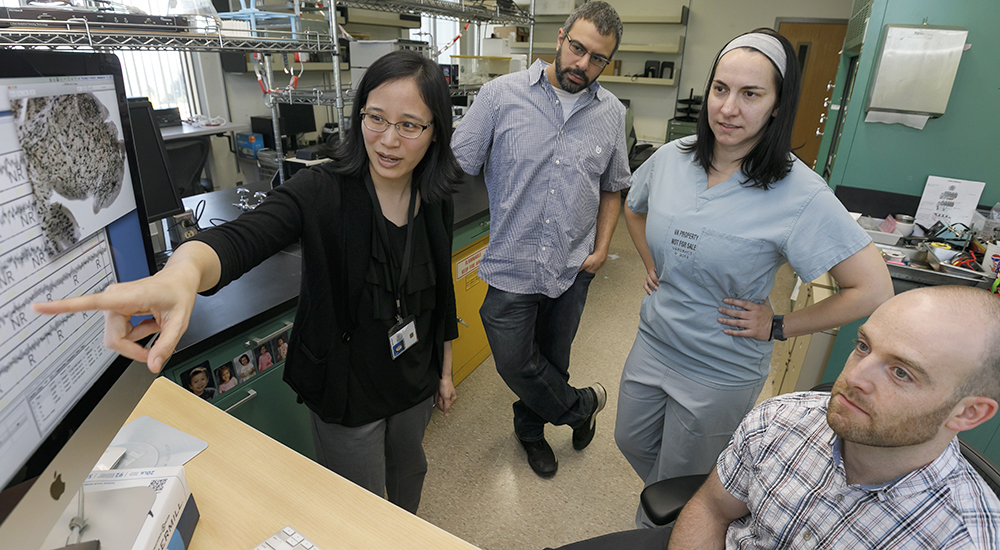
Pictured above, Dr. Lim and team members view an image from their sleep research lab in this pre-pandemic photo.
*How to join a research study (updated 3/3/21)
If you are interested in joining one of our research sleep studies, please visit https://sharp.pvarf.com and click on the “Join a study” page. A few of our studies can be done 100% remotely now. If you are interested in exploring other VA-sponsored studies, more are listed on this general website: https://www.research.va.gov/for_veterans/default.cfm.
Note: While there may be potential benefit from the intervention tested, joining a research study is not the same as clinical care. The main goal of a research study is to help evaluate and improve new treatments for sleep problems in Veterans.
Jewel Luckow is a VA intern with VA Research Communications. Photo by Kristyna Wentz-Graff. Wentz-Graff is a multimedia journalist at the Oregon Health and Science University.
Topics in this story
More Stories
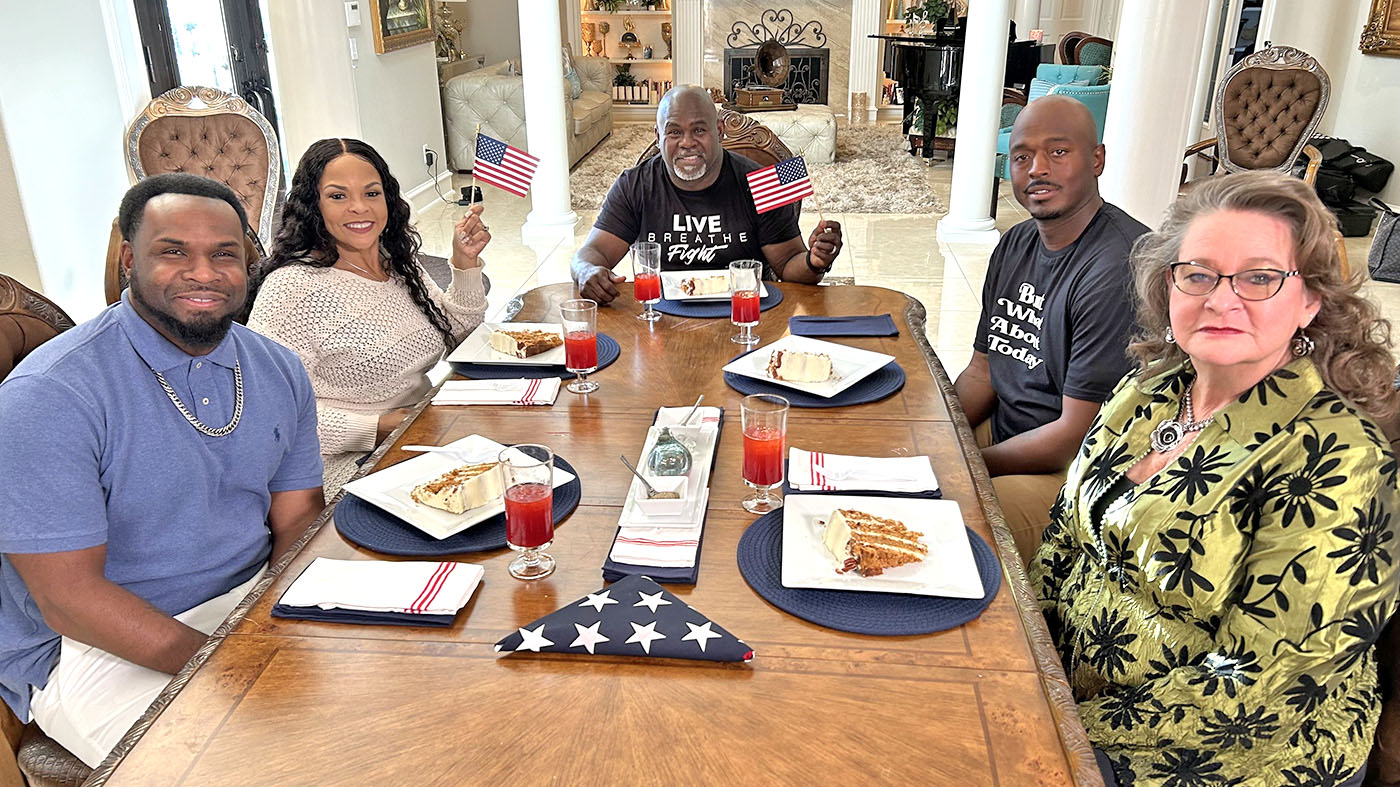
Mann Family Dinner episode discusses resources to address many of life’s challenges through VA’s Don’t Wait, Reach Out campaign.
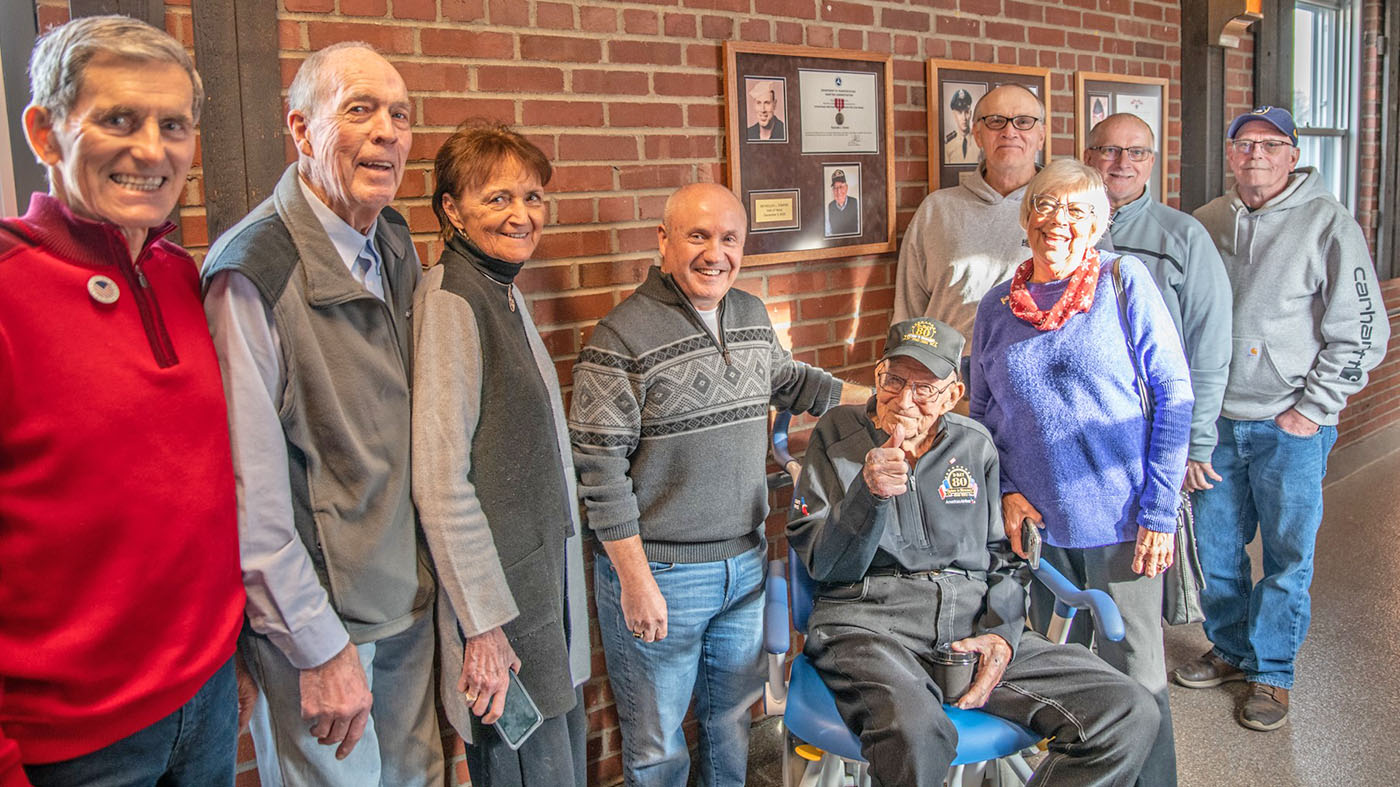
Teenager Mason Michaelson wanted to auction rabbits. His grandfather, a World War Two Veteran, suggested he give back to Veterans.
Veteran Reynolds Tomter, an inductee in the Hall of Heroes, served in the Merchant Marines in WWII.




“Thank you to everyone here who bravely shared your personal journeys with our community. It goes without saying that you are not alone in your struggles. It is our challenge at VA to come up with a better understanding of why, how, and what can be done next. If you need help, the first step (if you haven’t already) would be to contact your VA primary care or PACT team – if you need assistance with this, please reach out to your local patient experience coordinator.
“If you are interested in joining one of our research studies on sleep in Veterans, please visit https://sharp.pvarf.com and click on the “Join a study” page. A few of our studies can be done 100% remotely now. If you are interested in exploring other VA-sponsored studies, more are listed on this general website: https://www.research.va.gov/for_veterans/default.cfm
“I do want to emphasize that while there may be potential benefit from the intervention tested, joining a research study is not the same as clinical care. The main goal of our research studies is to help evaluate and improve new treatments for sleep problems in Veterans. Thank you again for sharing your comments.”
on behalf of Dr. Miranda Lim
I have severe sleep apnea along with RLS which makes it even worse. Would love to get into one of these studies. Tried the CPAP several times and either can’t breathe or they give me sinus infections.
I’m a retired veteran, 100% service connected disabled that served on active duty for twenty two and half years. During this time I had two different sleeping disorders: Narcolepsy and Sleep Apnea. I was going to different military doctors, clinics, and hospitals telling them about my sleeping problems. They would say I’m only fatigue and get more rest. I was never diagnosis with either of these sleeping disorders on active duty in the Army. When I retired from the Army and started going to the veterans hospital then the VA diagnosis me with both sleeping disorders. Now there part of all my VA medical service connected disabled disabilities. My other disabilities are: PTSD, ADHD, Migraines, Sexual Dysfunction, Degenerative Disc Disease and Arthritis Lower Back/Neck. And I have other disabilities. I had all kinds of problems in the Army because I was not properly diagnosis with all my medical disabilities. I truly believe by not being properly diagnosis during my active duty time in the Army caused me to have very serious problems serving on active duty and forced me to retire. I would like doctor Miranda Lim or someone from her staff to please contact me about my sleeping disorders. I want to know more about her research study and if she knows of any research study sleeping disorder programs I can sign up to be in? I hope my email message will help other veterans with their sleeping disorders.
I believe there are definite links between Agent Orange exposure, tinnitus, hypothyroidism and Parkinson’s like symptoms. Sleep apnea is tied either directly or indirectly to all four. Someone needs to research this in depth as the VA has been long remiss in helping Vietnam veterans. I would volunteer to be in a study on this…
i been having problems falling a sleep since boot camp at age 17,on ship for over 3 years trid drinking myself to sleep,that was the adviceof my chief petty oficer ………i wonder if theer is help ,im from whiting new jersey its near tons river and brick.
bob lerner
How do I apply? I have GAD. IM A Viet Nam Era Vet with GAD.
I wonder why this sleep study does not include tinnitus as a cause of sleep problems. The VA knows tinnitus has many secondary issues, to include sleep apnea, depression, anxiety, PTSD, excessive daytime sleepiness, headaches, memory loss, fatigue, and irritability, You also lose your ability to work.
i have sleep Apnea but i cant sleep proper with or without my mask i`ve tried the nose and also the face mask now with the full face mask no help i just cant sleep with the mask i wont go to sleep i try for a few hour but wont sleep i do sleep with out it but only a few hour what can i do to sleep
I served in Viet Nam, and was exposed to agent Orange. I have both sleep apnea and restless leg syndrome (bad). I get medication from V-A, which I’m thankfuil for, but still don’t get a good nights sleep, most of the time.
I take puritans Prides Black currant oil and stops my wrest-less legs within minutes of taking them
535 mg and they help with sleep.
Falling asleep is easy as long as I’m watching boring tv and laid out on my “lazy boy,”,but as soon as i get up and go to bed,thats where it goes bad. I know I’m tired but the brain stuff starts being active and getting too sleep is not possible, I can’t get to sleep sometimes till dawn.
I have PTSD
a but the trazadone I get does not work? Help .
I am 76 ,
JMB
USN 61-67
I’ve been diagnosed with PTSD and haven’t had a good night’s sleep since returning from Vietnam. I typically go to sleep at 11:15 or so and usually wake up after about 4 hours of restless sleep and generally can’t get back to sleep again. I went to the VA facility in Walla Walla for a sleep study. They wired me up and I spent the night. After waiting several months for the results I finally received a letter with the one-line diagnosis, “Patient has disturbed sleep patterns.” Not very illuminating.
I have dealt with sleep problems and ptsd for forty years. I was diagnosed with PTSD anxiety disorder depression insomnia, and it took the VA eighteen years before they would even acknowledge my diagnosis. I felt abandoned after seeking help, and then I was issued medications that would make me feel like I was in a fog. I felt helpless all the time, so dope up couldn’t function. Now I will stay up for two before I go to sleep. Only to sleep may two too three hours.
Forget and do not post my last comments. I had just finished watching Platoon and was just reading things in my mind. I know that you guys are doing the best you can. Thanks.
Where can we access Dr Lim’s research study reports? Would like to know findings. Is her research limited to the Portland OR VA area or does she involve participants outside that region?
There are definitive links between Agent Orange exposure and hypothyroidism and Parkinson’s like symptoms. Sleep apnea is tied either directly or indirectly to all three. Someone needs to research this as the VA has been long remiss in helping Vietnam veterans. If you push it off long enough, the problem goes away even though many veterans have suffered over the past fifty years because of their service unappreciated as it was. Just another reason, in retrospect, that I should have gone to Canada where they don’t kill off their young men over needless and senseless wars.
I would LOVE to be a study subject. I SUFFER with Sleep issues, PTSD, migraines, mild TBI, fibromyalgia and struggle with enough rejuvenating rest. Night sweets, that causes a barrage of issues the following day!
ME/CFS patients have been clinically proven to have the same functional profile as TBI patients. Has the VA addressed thus issue? I have a friend recently diagnosed who is being treated for TBI by a neurologist, who is doing well on his prescribed Indomethacin.
Used to sleep good probably during last few years in service had trouble have knocked my head a few times in service due to being a mechanic. Been diagnosed with osd sleep apnea was overweight a little always sleep on my side but still struggle with sleep I use my machine every night and now take melatonin to help keep me asleep have no trouble falling asleep have lost weight diabetic with hypertension and depression I also have tremors throughout my body that none seems to know anything about
I have those tremors too. I has a Cat Scan before I went in the Army but I haven’t been able to sleep without help for, well since I got out. I tried Melatonin, wasn’t enough. I know take Tylenol PM and my tramadol, that’s for my back, spinal arthritis. The tremors though I do know about. They just come on all of a sudden.
Glenn, I had Non Essential Tremors start about three years ago out of the blue! Being treated with Primidone until last August and then lorazepam was added for severe tremors which settles me down to sleep or drowsy!
Bottom line is I work part time and usually end up being picked up at work due to severe tremors! So out of my schedule M – T for 4 days working 9 a.m. to 2 p.m. with 1/2 hour break each day, I lose parts of a day or full days!
Just part of my story
I suffer tremors and lose 3 to 6 days a month working parttime Monday through Thursday for 4.5 hrs a day.
I’d be the first in line to do a trial study…
Sleep, what’s that?!? Sometimes I go for a day or two or even three days and during that time I get on average two hours of sleep in each day that I have a problem sleeping. I have a CPAP but getting supplies for it through the VA So I can or atleast try and get a good night sleep!! I mean I have anxiety which I’m on 200mg Zoloft, 3400mg gabapentin that doesn’t work anymore! Abilify, amytriptolin just to name a few! it’s like the VA puts a bandaid on a artery that’s just about bled out!!! I’m getting upset and disgusted with the VA. I’m gonna farm myself out to the civilian sector!
I need a report and to keep posted about this study please. I, too, am affected even though my Complex-PTSD-Childhood stems from my earliest childhood, uninterrupted.
Personally, I Believe MANY Veteran Females -especially older females- are Survivors of Childhood-originated PTSD. It is an underlying catalyst toward joining for many older females, is my personal belief.
3 to 4 seems the max time year after year, , I AM SURE THE SATILITE SYSTEM HAS EVERY THING TO DO WITH SLEEP DEPRIVATION.
I have been suffering from PTSD, insomnia, depression, anxiety, pain and sleep apnea with no compensation or relief. Served in the Army 70-72 Armored recon and the Marines 77 84 Battalion Admin chief.
Why won’t you post my comment? I’m 100% PTSD connected for MST, I managed for years but the symptoms continued to worsen over the decades until they took over and pretty much destroyed my life. 24 years ago my doctor added trazadone just so I could fall asleep and that did work, I can fall asleep with trazadone most nights, but that is where it ends. My sleep is so broken that I never get a full night’s sleep anymore. I wake every hour or two. Many times it will be an hour or more before I can fall back asleep. I’m always exhausted in the morning so I end up sleeping until noon. Of course I’ve tried forcing myself up early in the hopes that I would be very tired and sleep better at night. It doesn’t work and after several days I become a really angry person. I’m trying marijuana now, I think I need some that has more indica properties because this one isn’t doing it. I don’t want to use drugs at all for this, I’m on five meds now because of my heart and the unrelenting pain of a crushed L5 vertebrae plus advanced arthritis, I hate being medicated. I’m also using Ketamine because I am very depressed and highly…. I wish something in my body worked correctly because that light at the end of the tunnel is still a d ucking train.
[Editor: Please don’t post your comment six times, the blog thinks you’re spamming. All comments go into moderation queue and I manually approve them – or delete the spam.]
Go to bed when tired and then can not go to sleep, also if and when iI go to sleep I can not stay asleep.
Takes all night too fall asleep
No Doctor has helped me resume sleep for 15 years. Want the inside failure of VA HEALTHCAR, contact me. I don’t expect to hear from you, usually only tooting their own horns on how great they are. Reach out to me if your serious about a solution of sleep disturbances
I am 39 year old veteran. I have PTSD, a sleep disorder, and many other disabilities. I sleep walk on a regular basis. Sometimes I wake up in places and have to call my wife to come get me. Sometimes my phone is not with me and I have to stop and ask someone. I have asked the va for help and what resources they have to keep me in my house. They wanted to put me in the psych ward. Absolutely not. I lost trust in talking to the va about it. Because I tried asking for help more than once and each time I was asked, and threatened to stay in the psych ward. It is a constant battle. I’m very interested in this research
How Can I sign up for this Study I certainly have insomnia. I would very much like to participate.
I have Parkinson’s and I am being treated for PTSD
Have you ever heard of PTSD causing Narcolepsy?
That’s interesting, I want to follow to also see. Have you seen anything about the H1N1 vaccine is tied to narcolepsy. I’ve seen info about that.
As a combat Veteran from Nam I can tell u finally I sleep much better on oxygen through VA and more importantly feel much better in morning throughput day maybe that is answer
Major Depressive Disorder is sleep apnea connected to MDD?
I have several violent dreams a month. I’m afraid that my I might hit my wonderful wife during my swinging arms episodes. How should I pursue help?
I have a problem sleeping. I snore a lot. I wake up tired sometimes like I never had any sleep. If I wake up during the night I have a difficult time falling back to sleep.
I suffer from sleep disorder. I have a CPAP and it helps, but I am still waking up (To go on Watch) multiple times a night. I did a Stanford sleep study that was focused on lack of sleep and suicide caused by lack of sleep. I am not suicidal I just wanted wanted help sleeping. I would love to find more help to be able to sleep through the night.
I’m suffering with sleep apnea and can’t seem to avert the problem. I also suffer with ptsd . It’s not getting any better. Getting zero compensation what do I do?
What state do you live?
Joel, I too have both ptsd and sleep apnea. I finally reached to my VA rep and she diagnosed me with PTSD first and is now working on adding sleep apnea as a secondary for my disability.
Cant go to sleep at night I’m always thinking what could go wrong if or when I might get attacked around 4 in the morning or when its turning day light I feel the threat level is down and I sleep.If I do sleep I’m awake every hour on the hour
Shortly after arriving in Iraq I started taking Tynelol PM to sleep. There was always mortors and small arms fire throughout the night. After getting home, I was diagnosed with PTSD and TBI. I’ve been prescribed many different medicines. Right now I am taking prescribed Trazodone and Melatonin for sleep and others for PTSD. The Traz and Mela help, if I’m not super alert. I have a very difficult falling asleep and staying asleep. My body is conditioned to stay up until I’m falling asleep. I’ve come to the belief that it is because “bad things happen(ed) at night.” I wake up once to use the restroom. Then I wake up 3-4 times for different reasons and different lengths of time. I was diagnosed with sleep apnea one year and the following year I was not diagnosed with. I’ve sustained trauma and this sleep issue is a problem. I am tired most of the time. Thank you for reading this.
I served four years in the Navy with a sleep disorder. It hadn’t been diagnosed but I knew something was wrong. My sleep disorder started when I was around 18 years old. I trained myself to appear like nothing was wrong or different when my mind would slip into what I called a state of twilight awareness. I trained myself to be able to walk and give simple short responses when in this state of twilight awareness. No one ever suspected this was happening to me. I couldn’t explain it when I tried I was told I wasn’t getting enough sleep and that I need to go to bed earlier!!! Right! It did start to get worse as the years went by because I began to lose more and more productive wakeful hours in the day! Finely when I was 36 I demanded my PCP doctor find someone that could help me and not a Psychiatrist since I was already seeing one! My PCP referred me to a new Sleep study clinic at Boston Medical Center. And I was diagnosed with Idiopathic Hypersomnia. Since I was already being treated for Adult ADHD with an Amphetamine medication the only thing that could help was to up my daily dose. Then in 1999, a new drug was released on the market for the treatment of sleep disorders and Narcolepsy. This drug is Provigil. I will never forget the day I took my first dose. It was like someone lifted the fog off of my life! I stayed awake for the whole day. I didn’t have any moments of my brain slipping into twilight awareness. I remained on that medication and then was switched to Nuvigil when it was released which is a much better version of this drug. So I have been on this medication for just over 20 years now and the only time my brain slips into that twilight awareness is if I miss a dose of the medication. I had lived at least 18 years of my life in a fog!! So for me, this medication has been a lifesaver. And I strongly suggest that if anyone out there suffers from what they believe is excessive daytime sleepiness that they talk to their doctor about having a sleep study done. There is no reason these days to live your life in a FOG of sleepiness!!! Oh, BTW I have never put a claim in for my sleep disorder because I knew before I joined the Navy that something wasn’t right. And as it got worse I most certainly was not because I was in the Navy. I just wanted to make this clear for anyone who might think I would ever file such a frivolous claim with the VA. And I am not saying that Veterans don’t develop sleep disorders while on active duty. I know nothing about that. I have just related my story about my sleep illness and how I got help for it. And a significant part of my story is that years ago it use to be very hard to get anyone to understand the issue regarding excessive daytime sleepiness. Especially while in the service. Think about how many times you might have to do a 24-hour watch then go right one to perform your regular workday!!! Well of course you’re going to have a bit of excessive daytime sleepiness that day!!! But what happens when it doesn’t go away??? Years ago you were threatened with being charged with malingering!!! And told to get your ars back to work!!! Times have changed so there is more of an understanding that those strange symptoms might really be something that needs a closer look!
Sunosi is a more recent medication, which I used to take, but it made me a little bit irritable so I stopped taking it. I still use my C-PAP though. Narcolepsy has to do with the (lack of) production of orexin hormone (hypocretin) in the brain. There is supposed to be a new drug coming out (or maybe it has recently already come out) for regulating orexin even better than Sunosi.
I’m very interested in knowing the link between ptsd and sleep ascension I presently suffer fm ptsd from combat duties in viet bam put in a claim for sleep acucma in relationship to ptsd and was denied as va said that there is no relationship to ptsd would like a clarification on this tks
Thank you for your story. I will definitely take your advice on being referred to a sleep study. I’ve had daytime sleepiness so bad I lost a job I loved, got into a car wreck (thankfully it wasn’t serious) but my young daughter was in the car with me and I’ve been fighting daytime sleepiness for decades now.
I wake up during the middle of the night and can’t get back to sleep.
Please provide additional contact information for VA patients outside of Oregon on how to apply for this program.
I have a hard time falling asleep. Its getting to the point where not even the sleeping pills are working. Where can I get help?
How does a veteran find out about signing up for the Sleep Study Disorders, to include PTSD. I definitely need help in this area by VA, or civilian. I am 100% disabled.
You can make an appt at ur local va. They have a sleep clinic
The sleep problems mentioned in this article mirror my personal sleep problems. I am on disability for TBI among other things and have never been aware of any VA action addressing this problem. I would like to know how this study might affect me, as I am now 80 years old with no relief in sight.