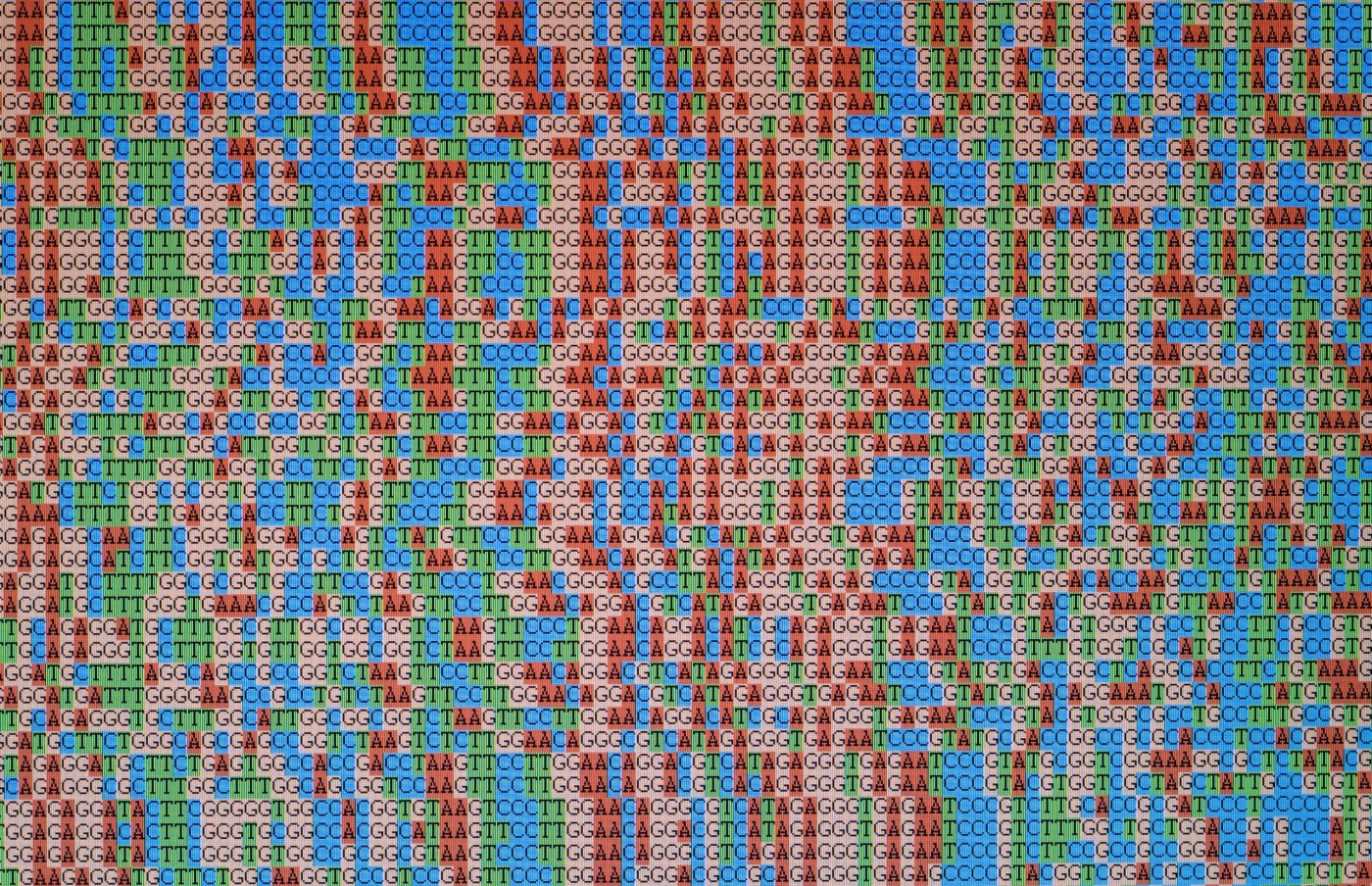
MVP has created whole genome sequences for over 140,000 Veterans. However, it takes time to process this large amount of data and make it available for research.
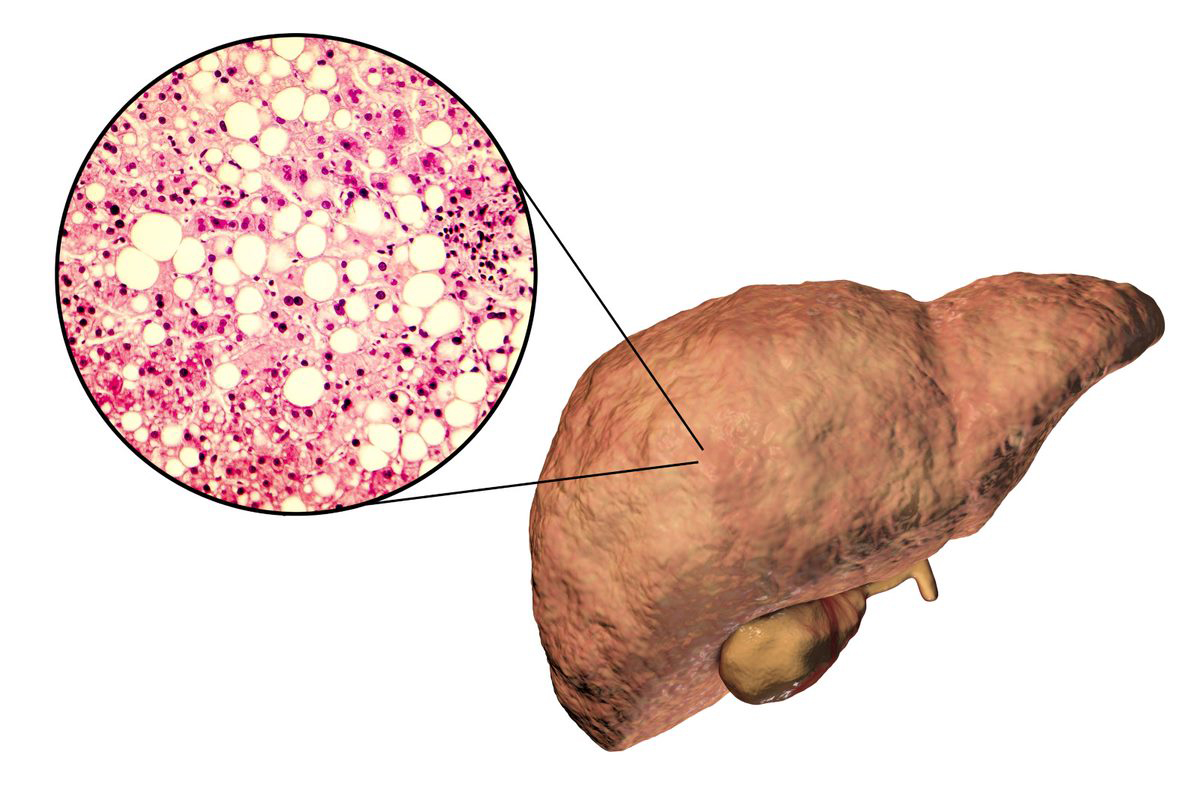
NAFLD is a growing cause of liver disease. It has an estimated worldwide prevalence of 25% in adults. In the United States, that prevalence is projected to climb to nearly 34% by 2030.
Standing Ready highlights the significant contributions – past, present and future – of the VA health care system through a historical lens.
Height is not typically considered a risk factor for diseases. But past research has shown correlations between how tall someone is and their likelihood of experiencing a number of health conditions. What isn’t well understood is whether this correlation has a biological basis or is due to other factors.
The study involved genetic data on more than 300,000 participants of VA’s Million Veteran Program (MVP), along with more than a million subjects from other biobanks, including 23andMe. With such a large participant pool, the researchers were able to spot trends in genetic risk of depression not previously known.
VA's Precision Oncology program has significantly grown over the past several years and today is used in almost every VA oncology practice nationwide.
Research based on VA’s Million Veteran Program has identified multiple locations in the human genome related to the risk of re-experiencing traumatic memories, the most distinctive symptom of PTSD.
A physician-investigator at the Washington DC VAMC is a member of the African American Cardiovascular Pharmacogenomics Consortium, created in 2016 to advance precision prescribing—based on patients’ genes—of cardiovascular drugs for African Americans.
The Million Veteran Program is research that hopes to understand how genes affect health. The largest database of its kind in the world, it will answer important questions affecting Veterans’ health.