A group physical therapy program by VA Geriatric Scholar Ralph Magnuson and colleagues from the Redding VA Clinic in Northern California combines exercises with instruction on the neuroscience of pain to help older Veterans increase mobility, reduce chronic pain, and improve quality of life.
Pain neuroscience education (PNE) is a way of understanding the brain’s role in producing pain with the aim to decrease the severity of how patients perceive chronic pain.
Traditionally, physical therapy falls into a biomedical model of care, explained Dr. Magnuson. “We assess that shoulder or back and try to identify the pain generator. When we find it, we try to fix it. Therapeutic neuroscience is more on the bio-psychosocial model where we focus on the whole person.”
At the start of the program, Magnuson asked participants about their pain management goals. “We’re moving towards patient-focused goals versus the primary care physician or therapist-driven goals.”
Veterans told him, “I just want to walk with my grandkids,” or “I want to be able to go out to dinner with my wife and shop in the community,” and “I want to know if there’s anything else I could possibly do.”

Physical therapy helps older Veterans increase mobility, reduce chronic pain and improve quality of life.
Engaging patients in their own care
Before and after the program, participants were assessed for the presence of chronic pain and its intensity to test the effectiveness of physical therapy combined with PNE. Average pain scores improved for all participants by more than 20%.
“We saw a significant change as a group. When they worked together, with camaraderie that was exercise-based, they just in general felt better,” Magnuson explained. “They were observed moving better. I think that relates to, If I feel better, and I move better, my pain must be better.”
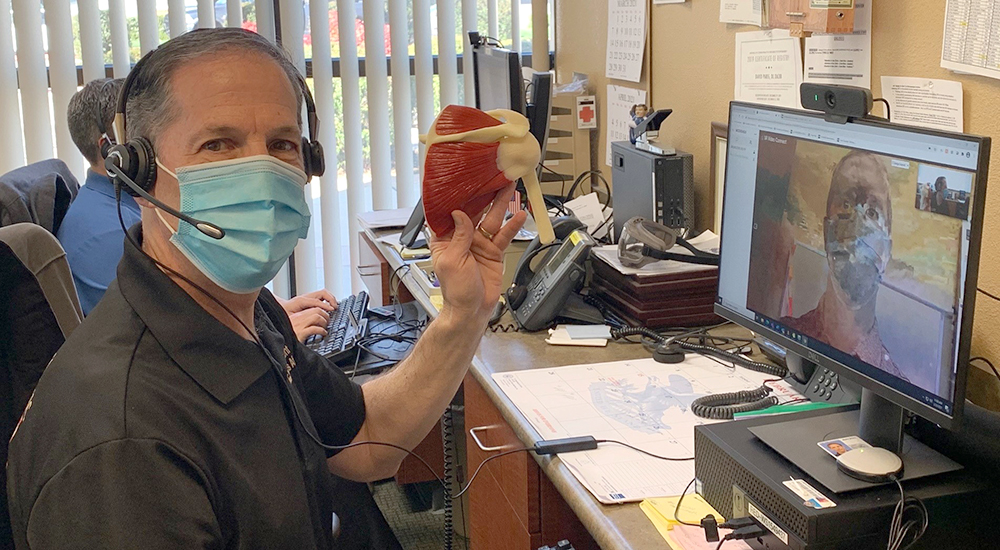
Magnuson encourages Veterans to commit to exercise after the program to maintain improvements. Though COVID-19 physical distancing measures at the Redding VA Clinic gym have temporarily halted group physical therapy, he helps patients stay active using VA Video Connect. He also delivers virtual therapy to rural Veterans in Yreka, Mount Shasta, and Burney.
Pictured above, Magnuson conducts a physical therapy telehealth visit for a shoulder impingement and rotator cuff condition.
Telehealth consultations with specialists for Veterans in rural areas
When patients with chronic pain need advanced care, Magnuson uses telehealth to connect patients with Kathryn Schopmeyer, Physical Therapy Program coordinator for Pain Management at San Francisco VA Medical Center.
Schopmeyer is a nationally recognized PNE specialist who collaborates with physical therapists throughout VA Northern California Health Care System. “The three of us work together. I’m a local resource for that patient instead of them having to drive to San Francisco,” she said.
VA Geriatric Scholars Program
Magnuson’s program was inspired by and developed as part of his engagement in the VA Geriatric Scholars Program Quality Improvement Workshop and Practicum.
The Geriatric Scholars Program is a national workforce development program that trains primary care providers in geriatric medicine and teaches fundamental skills in quality improvement based on the IHI Model for Improvement and PDSA Cycle.
Magnuson’s experience with the VA Geriatric Scholars Program led to another quality improvement opportunity. He joined the coaching program within VA known as VA Transformational Coaching Network. “It’s a way to give back. We’re paying it forward and helping somebody else get to the end result like I did.”
Maureen Jerrett is a communications contractor for the VA Geriatric Scholars Program.
Topics in this story
More Stories
Watch the Under Secretary for Health and a panel of experts discuss VA Health Connect tele-emergency care.
The 2024 National Veteran Suicide Prevention Annual Report provides the foundation for VA’s suicide prevention programs and initiatives.
Theranostics is a specialized field of nuclear medicine that uses a two-pronged approach to diagnose and treat cancer.






Shortly after the pandemic began I dislocated a shoulder. In see a nurse at a VA clinic, I was informed it probably was a torn rotator cuff. For ten months I suffered pain. I knew it was not what was off the cuff (pin intended) and not scientific fact.
One day I decided to see if I could resolve the shoulder myself. Pop, crackle, the bones re-aligned themselves and no more pain from that.
Instead I had pain from a COVID shot, probably needle hit a nerve. Again, not much help until nurses changed and then I finally was referred for therapy.
Where can I find a list of locations where this program is active?
I taught HOW TO LIVE WITH CHRONIC PAIN at the VA in Providence, Rhode Island. We stopped after ten sessions for lack of attendance. It was offered but not taken. I use what I learned in the class. Check with the Providence VA to see if they still have that program.
My husband served over 20 years in the military. He’s now 65 retired, and now we find ourselves battling the common notion that pain medication is now socially unacceptable. No matter the injuries a veteran may have that was incurred doing their military career. Yes, we know and understand the widespread misuse of prescription drugs! Yet, there should be a solution for those patients who are in pain and need the medications to live as pain free as possible. No two people should be treated the same. Nor should a blanket effect over no prescription medication issued be placed on every veteran. Our husbands, deserve better and I see the pain and discomfort he suffers, the doctors do not. With diagnosis of injury, it should be the”patient” choice and their doctor to come up with a viable care plan, not just the VA system in general
You must enlist the help of as many people at the VA as possible, ie. nurse, patient advocate, social worker, complaint forms, etc. I’ve been fighting for my care since 1992 and it never ends. I find employees who truly care and are willing to help and I’ve found those who couldn’t care less and do absolutely nothing to help me. I suffer chronic and severely with muscle pain, nerve pain and skeletal pain. My doctor is late filling my monthly opioids prescriptions 90% of the time. This has been an ongoing problem for 10+ years! The VAMC does not care that he does this to his patients. It’s unbelievable but the truth. Please keep fighting for your husband. Chronic and severe pain is just awful!
The VA people I have encountered often seem to think that I am taking advantage of our Government. This seems to be a condition that many veterans feel. Nothing will change until you do.
Yes we have encountered this same attitude
Until you instruct your employees that WE Veterans are to be helped, not distrusted we will continue to have problems.
There needs to be “ongoing” PT programs for veterans that have chronic pain as I do. I have been to numerous PT sessions but they aren’t “ongoing” and that’s the problem. Going, stopping, going, stopping, etc., etc., doesn’t accomplish anything!
VA should contract out PT programs to local providers that are there in the neighborhoods of ailing Veterans.
I have done PT but it didn’t seem to help. Is this program different and is it offered at the VA in NM in Albuquerque.
My husband has parkinson’s and needs pain management to relieve the overwhelming pain associated with constant shaking. we have had in home PT thru Medicare but that’s about to run out. once Medicare is done there will be nothing. Is there a VA program in Charlotte,NC like the bio psychosocial model mentioned in this article? Or is there ANY form of Physical therapy in Charlotte for Vets.
I am a 100% P&T veteran who is receiving pain management treatment through CCN. Physical therapy is a luxury and is not authorized unless there is significant effort (Begging) for it. I know that it keeps me more mobile but my opinion obviously does not count. I guess that I am expected to get rid of furnishings in my home to make room for exercises learned… I guess I will have to use my private insurance and pay the $30 per visit copays for a service related injury…
I am very interested in such a program for myself. I would not be able to go to my nearest VA hospital in Loma Linda and would need therapy close to my home in Hemet. I am an 87 yo Air Force Vet and would like to increase my mobility safely. Right now I have an unsteady gair. Using my new treadmill gave me severe muscle cramps. Is is possible to set up a program for me such as described in this blog but in my local area?
This is important for all veterans. For a long time I received pelvic traction at what is now Lake Baldwin VA in Orlando. Then one day I was told by the person in charge of the PT department that I could no longer get it, even though I was a priority one veteran. Not long after that I had to stop working due to uncontrolled low back pain. The loss of PT had a significant negative affect on me.
I am sorry to hear that you could not receive in person pelvic traction treatment after finding it helpful for your low back pain. The VA will pay for you to receive a home lumbar traction device if the in clinic treatment was helpful. Check with the physical therapy Dept. at your VA and ask to have the Saunders home lumbar traction device delivered or issued to you.
Christian Wyman, DPT; Coatesville VAMC, Coatesville, PA 19320.
Wont publish my comment on how bad the VA has messed me up prescribing me excessive amounts of oxycodone.
Physical therapy, lol. The Pain Management Clinic here at Carl Vincent (Dublin, GA) has been shut down forever waiting to hire a doctor to run the clinic. I have to drive 3 hours to see a pain management doctor who tells me the VA screwed me over by prescribing excessive doses of oxycodone instead of fixing the problems. The VA is a plague.
Does the VA offer in-home PT? Nearest VA is in Loma Linda, California.
When will it come to Alaska?
Are your physical therapy departments open at this time with the COVID-19 virus playing havoc in our various communities? I’m living in southern Oregon near White City where we have a large Veteran community due to the long standing veteran rehabilitation facility currently called the SORCC.
It’s been difficult trying to get help at the sorcc weather ones needs may be physical therapy or in optometry due to the COVID virus causing mass shut downs there making many veterans in & around the community go without the care they need.
It appears to me to be overkill as far as the many departments closed like physical therapy & optometry & the fact that if a veteran needs drug & alcohol Tx, they are confined to a room approximately 6ft by 12ft for about 10days. And this is why I ask if your P.T. Dept’s are currently open as it appears in this e-mail you have added your program to. Thank You! Sincerely, Another half blind & aching, frustrated veteran
The P.T. in Redding, California where Dr. Magnuson works is open but they see fewer Veterans than what was seen before COVID.